In the fight against cancer, cell and gene therapies offer many new possibilities. They are revolutionizing cancer treatment by harnessing the body’s own cells to combat the disease. At UMC Utrecht, our researchers are at the forefront of these advancements, translating laboratory discoveries into clinical applications that benefit patients directly.
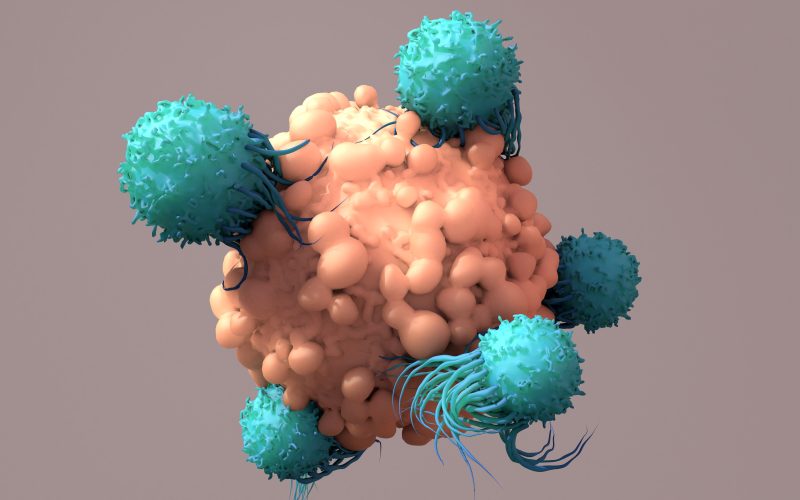
Cell therapy involves using living cells to treat diseases. In cellular cancer immunotherapies, we take immune cells from a patient, multiply them in the laboratory, and place them back in the patient. By doing so, we strengthen the immune system’s ability to target tumors. We use gene therapy when patients lack tumor-reactive immune cells. Then, we modify the immune cells to improve the tumor-fighting capabilities of the cells.
Better equipped T cells
An important type of immunotherapy is CAR-T cell therapy, which combines elements of cell and gene therapy. This treatment boosts a patient’s immune system to fight cancer by genetically modifying T cells, a specialized type of immune cell. T cells are first extracted from the patient’s blood. In the laboratory, they are modified using a so-called ‘viral vector’. This is a safe piece of a virus, helping to insert new genes into the T cells. The newly created genes encode information for a specific receptor, known as CAR, which recognizes and attacks cancer cells. As a result, the T cells are better equipped to target and destroy cancer cells.
Testing ground
“CAR-T cell therapies play a vital role in current research and our daily clinical practice,” says Jürgen Kuball, professor of hematology and head of the hematology department at UMC Utrecht. His research group focuses on the immune system’s mechanisms for attacking cancer cells and advancing methods to modify immune cells.
Cellular gene therapies with CAR-T cells are now standard healthcare in most academic centers in the Netherlands, particularly for different forms of lymphoma and leukemia. The challenge now lies in expanding these therapies to a broader range of hematologic diseases (blood disorders) and solid cancers (compact tumors originating in organs or tissues). Additionally, treating autoimmune diseases with cellular gene therapies has shown spectacular clinical responses. “Hematology is often a testing ground for new developments: you have relatively easy access to the cancer cells and can selectively generate and find cells. Therefore, our mission is to make the next steps to more challenging diseases”, Jürgen notes.
“All patients have the right to receive the best treatment, even if they have a very rare form of leukemia”
From research to clinic
Trudy Straetemans is associate professor of tumor immunology at UMC Utrecht. She develops new cell and gene therapies to improve cancer treatment. Furthermore, she leads clinical translational research efforts to bring such innovative laboratory findings to patients quicker.
Trudy explains: “Imagine, we’re building with LEGO, creating constructs aimed at attacking cancer cells. By experimenting with different LEGO block combinations, we identify the most promising options. However, translating these novel innovative therapeutic strategies from the laboratory concept into first-in-human clinical trials is a most challenging and frequently completely underestimated phase of development. Our goal? To find effective therapies that can be expanded in larger studies. With this approach, we’re seeing increased success in clinical practice, making a real impact for cancer patients.”
National collaboration
To speed up the from-lab-to-clinic process, Trudy, Jurgen and their colleagues have developed a national innovative infrastructure for cell and gene therapies: the Center for Advanced Therapies (ICAT), which is part of the RegMedXB national pilot factory and is supported by the Dutch National Growth Fund (NGF). In addition, all academic hospitals have joined forces in translational cell and gene therapy research through the DARE-NL consortium, with Trudy as the project leader.
“At DARE-NL, we focus on sharing knowledge and fostering synergy between centers and research groups,” Trudy explains. “Our aim is not to compete but to complement each other. DARE-NL enables the exchange of insights into advanced therapies.”
The Oncode Accelerator consortium also adds to these collaborative efforts. The Cell and Gene Therapy platform within this public-private partnership is led by the Netherlands Cancer Institute (NKI) and UMC Utrecht. “We aim to speed up the development of new types of therapies so that patients will have earlier access to them.”
“We aim to speed up the development so that patients receive earlier access to this new type of therapies”
UMC Utrecht’s unique position
UMC Utrecht has a unique approach to cell and gene therapy. “Our strength is rooted in our own research and collaborations with institutes at Utrecht Science Park, like the Hubrecht Institute and the Princess Máxima Center,” says Jürgen. “With the Princess Máxima Center, we are developing a clinical study for children and young adults with cancer. Additionally, growth funds, such as RegMedXB, NextGenHighTech and Oncode Accelerator, have further strengthened our position and allow us to faster translate innovations into first-in-human clinical trials.”
Next generation: TEGs
UMC Utrecht also develops its own version of CAR-T cells: TEGs. These are genetically engineered T cells that combine the best of two types of T cells (alpha-beta and gamma-delta cells). “Our cells use a completely new mechanism to recognize cancer,” Trudy says. “They recognize cancer as a metabolic disease, targeting many different cancer types with one type of receptor.”
These special types of CAR-T cells are currently being developed, manufactured in our GMP facility, which is part of the ICAT, and tested in patients at UMC Utrecht. The current clinical TEG study focuses on adults with acute myeloid leukemia and multiple myeloma. The clinical study is in its early stages. The team is testing the TEG therapy on a small group of patients, looking for the highest safe dose.
“This allows us to discover how many of these cells we can safely use without patients suffering from serious side effects. It’s important to find the right balance between effectiveness and safety,” Trudy explains. With each higher dose, they treat a new group of patients. The results look promising. A patient with acute myeloid leukemia no longer had signs of the disease after treatment, lasting for six months. “This fills us with hope and shows that we are on the right track.”
“We strive for diversity in our methods, from PCR to organoids and AI”
Advancing TEGs for solid tumors
Solid tumors present a significant challenge in immunotherapy due to their complex microenvironment, which often hinders immune cell infiltration and function. That is, the solid tumors are being protected by their own sort of powerful ‘firewall’.
To address this, Jürgen and his team are developing second-generation TEGs by enhancing their ability to penetrate and act within solid tumors.
Dennis Beringer is assistant professor at UMC Utrecht. “By equipping TEGs with additional proteins, we aim to overcome the defensive barriers of solid tumors,” Dennis says. “This enhancement does not only improve their ability to recognize tumors but would also make it possible to use them with various cancer types, including breast and colon cancers.”
Preclinical studies have shown promising results. In mouse models, the enhanced TEGs effectively targeted and reduced tumor size without harming healthy tissues. “These findings are encouraging and suggest that our approach could lead to more effective treatments for patients with solid tumors,” Jürgen notes. “Translating such ideas into clinical studies would be not possible without dedicated physicians like Monique de Witte and Lotte van der Wagen, who are preparing and leading patient registries and clinical trials. It is a team effort, from the laboratory to the clinical trial, requiring complementary expertise.”
Lower costs with new techniques
As mentioned earlier, the UMC Utrecht researchers can transfer their therapies more quickly from the lab to clinical practice. “We’re able to make improvements at every step,” Trudy emphasizes. “That is also very important to make the new therapies more affordable. A CAR-T cell treatment is personalized: it is tailored to an individual. Cells from a specific patient are being used. This makes the treatment expensive and complex, but UMC Utrecht is looking for ways to lower costs.”
“For example, we would like to improve our production and selection processes: how can we make more T cells and pick out the best ones?” Trudy explains
Place genes more efficiently
Another way to increase efficiency has to with the so-called vectors involved. Mostly, viral vectors (safe pieces of a virus) are used to place a gene exactly in the right place. One way to work more efficiently would be to use non-viral vectors to genetically modify the cells.
“Being able to generate the vectors that allow engineering T cells is crucial”, says Zsolt Sebestyen. He is associate professor of tumor immunology at UMC Utrecht. “This is a truly underrecognized bottleneck, as we otherwise will never be able to test multiple innovations rapidly in a less expensive way.”
The UMC Utrecht researchers are also investigating new ways to accelerate the growth of cells. “And we strive for diversity in our methods. We apply everything”, Zsolt explains. “Such as PCR (polymerase chain reaction: using nucleic acids to rapidly make loads of copies of DNA samples – ed.). Also, we make use of 3D models, such as organoids (lab-cultured mini-organs – ed.). Furthermore, we employ single-cell sequencing (isolating and amplifying the genetic material of each isolated cell – ed.). And with the amount of data we have now acquired, artificial intelligence (AI) is also becoming increasingly important to quickly analyze the material.”
“This enhancement would also make it possible to use them with various cancer types, including breast and colon cancers”
Looking to the future
Looking to 2030, the landscape of cell and gene therapy looks promising. Trudy shares her view of the future: “We aim to have several clinical trials underway by then, and we hope to have started a new TEG study.”
Jürgen is also looking ahead: “I see us mainly doing innovative and small-scale clinical trials. The aim of our academic research is to be at the forefront of new developments. We set up our studies in such a way that pharmaceutical companies will be able to take them over and test them further with larger groups of patients.”
Jürgen, Trudy and Zsolt think it is important that academic hospitals also focus on diseases that are not so common. “We would also like to develop effective and affordable therapies for conditions receiving less attention from the pharmaceutical industry”, says Jürgen. “All patients have the right to receive the best treatment. Even if they have a very rare form of leukemia. We would like to be able to offer these patients a treatment that is not commercially available. For example, with our own CAR-T cells.”
At the same time, they hope to make CAR-T cells affordable for all patients.
But a challenge in cell and gene therapy is the current logistical model. “Now, we send the collected cells from patients to the USA for processing and then get them back for treatment,” Trudy says.
“We have set up facilities in Europe to facilitate this process. At the moment, the number of patients is still relatively small. But if we’re going to treat more patients in the near future, this logistical approach will have to be improved. Decentralized production at multiple hospital sites could be one solution, and academic hospitals in the Netherlands could become an important part in the production chain.”
What is cell therapy?
Cell therapy involves the introduction of healthy cells into a patient’s body to repair or replace damaged or diseased cells. These therapeutic cells can be sourced from the patient (autologous) or a donor (allogeneic).
By delivering functional cells to affected areas, cell therapy aims to stimulate the body’s natural healing processes. This approach is applied across various conditions, ranging from skin injuries to complex diseases, like heart failure.
With cancer treatment, cell-based immunotherapy utilizes immune cells, such as T cells, extracted from the patient. These cells are expanded in the laboratory and then reintroduced into the patient’s body to enhance the immune system’s ability to target and destroy cancer cells.
What is gene therapy?
Gene therapy is an innovative approach to treating diseases by directly modifying the genes within a patient’s cells, targeting the root cause at DNA level.
A major advantage of gene therapy is its potential to provide long-term solutions for genetic disorders or to establish a lasting defense against cancer. In some cases, a single treatment can offer long-lasting effects, reducing or even eliminating the need for ongoing interventions.
The effectiveness of gene therapy largely depends on the safe and efficient delivery of genetic material into the patient’s cells. Various methods, including viral vectors and non-viral techniques, are employed to achieve this.