UMC Utrecht is coordinating an innovative, international study within Europe to determine the best treatment of bloodstream infections caused by the bacterium Staphylococcus aureus. This research is urgently needed because also in the Netherlands – despite the best possible care – each day 2-3 patients die due to such an infection.
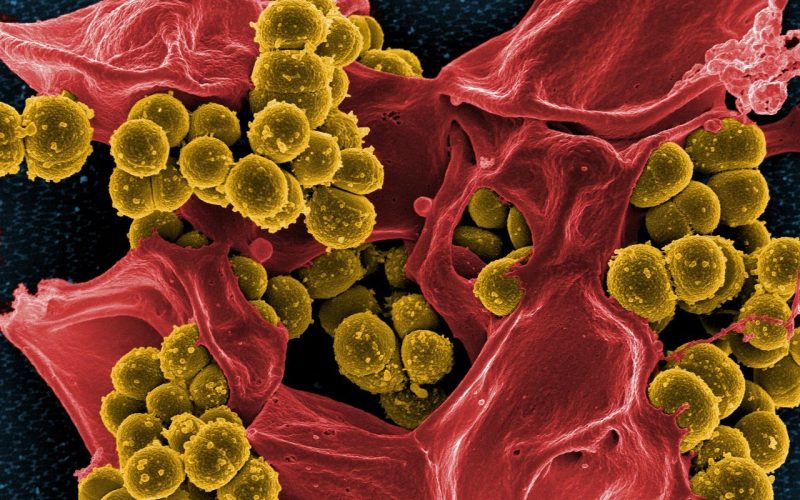
Staphylococcus aureus is a bacterium that lives on the skin or in the nose. Usually this does not cause problems, but sometimes this bacterium causes an infection. When it then enters the bloodstream, we speak of a “bloodstream infection” or “bacteremia”. Doctors often use the more specific term “Staphylococcus aureus bacteremia (SAB)”. Bloodstream infections with S. aureus are common worldwide and can have serious consequences for patients. According to a recent study, SAB occurs between 3,500 and 5,000 times annually in the Netherlands, with patients routinely being hospitalized and treated with intravenous antibiotics. Despite the best possible care, mortality due to SAB is high, and researchers estimate that 20-25 percent of patients with a SAB die within 30 days of infection (for the Netherlands, it means that 2-3 patients die each day due to a SAB).
Because of the potentially serious consequences, a SAB should be treated with antibiotics as soon as possible, and guidelines recommend a wide range of antibiotic treatments. However, it is not known which antibiotic (or combination of antibiotics), dosage, method of administration and duration of treatment works best. In the international S. aureus Network Adaptive Platform (SNAP) trial, physicians are investigating which antibiotic regimen works best as a treatment for SAB. In particular, they are looking at the chances of survival and recovery of patients hospitalized with such an infection.
“The SNAP trial aims to improve treatment outcomes in patients with S. aureus bloodstream infections”
In order to reach the desired number of at least 7,000 participants in the SNAP trial as quickly as possible, the study, which originated in Australia, was recently expanded to other parts of the world, including Europe. UMC Utrecht – led by physician-microbiologist Prof. Marc Bonten MD, PhD (professor of molecular epidemiology of infectious diseases at UMC Utrecht and CEO of Ecraid) and internist-infectiologist Marjolein Hensgens MD PhD (internist-infectiologist at UMC Utrecht) – will act as the coordinators for the trial within Europe. Both are also members of the international steering committee of the SNAP trial. Some parts of the research within the SNAP trial (such as the pharmacokinetics of certain antibiotics) will be conducted in close collaboration with Radboudumc. Execution of the European part of the study will be done by the European Clinical research Alliance for Infectious Diseases (Ecraid). In the Netherlands, a total of 11 hospitals will participate in the study.
Marjolein Hensgens, leader of the study within UMC Utrecht, explains: “The SNAP trial aims to improve treatment outcomes in patients with S. aureus bloodstream infections by reducing mortality and complications. In terms of design and scope, this innovative study is one of the first of its kind. The study is taking place in hospitals in Australia, New Zealand, Singapore, Canada, Israel, South Africa and recently also in the Netherlands. We expect other European countries to join soon.”
The randomized controlled trial (RCT) is the gold standard method for demonstrating the effect of a treatment. However, RCTs are expensive, time-consuming and can answer only a few research questions per study. To get around these limitations, adaptive platform trials (APTs) have been developed. APTs can answer multiple questions simultaneously using a pre-established infrastructure and a master protocol. As an APT progresses and more patients participate, outcomes can be analyzed at specific times in the interim. Researchers can then determine whether there is sufficient data to assess – according to predefined rules – whether the research question can be answered. If a studied treatment turns out to be better than the standard treatment, then that treatment can become the new standard. Also new treatments can be added to the study. With the APT design, a new internvention can be investigated quickly and cost-effectively.