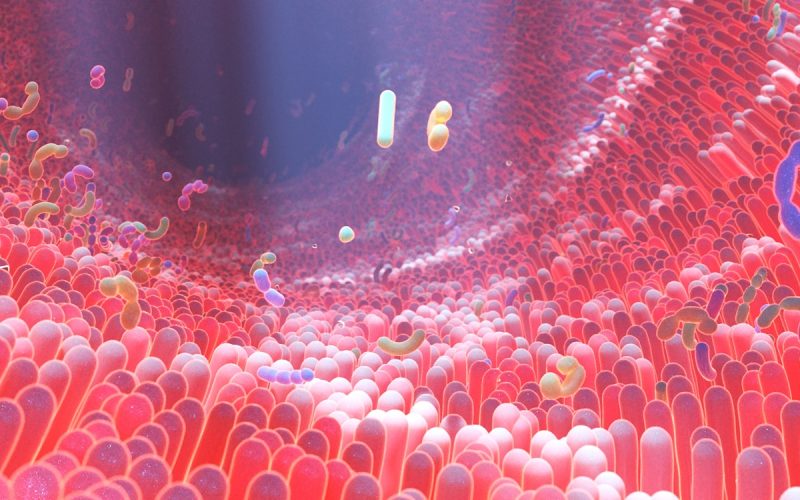
Bacteria in the human gut can directly deliver proteins into human cells, actively shaping immune responses. Led by researchers at Helmholtz Zentrum Munich, with participation from international partners including UMC Utrecht, the consortium has discovered this previously unknown mechanism of communication between gut bacteria and human cells. The findings reveal a new way in which the gut microbiome can influence the human body and may help explain how changes in gut bacteria contribute to inflammatory diseases such as Crohn’s disease.
Although the human gut microbiome has long been linked to immune, metabolic, and inflammatory disorders, most evidence is correlative, and the molecular mechanisms behind these connections remain largely unexplored. The goal of the study, which was published this week in Nature Microbiology, was to better characterize some of the underlying processes of how gut bacteria affect human biology. By systematically mapping direct protein–protein interactions between bacterial and human cells, it is now possible to suggest molecular mechanisms behind these associations.
Immunologist Marianne Boes, PhD
The study shows that many harmless, everyday gut bacteria possess type III secretion systems – microscopic, syringe-like structures that can inject bacterial proteins directly into human cells. Until now, these systems were thought to exist only in pathogenic bacteria such as Salmonella.
“This fundamentally changes our view of commensal bacteria,” says Prof. Pascal Falter-Braun, PhD, Director of the Institute for Network Biology at Helmholtz Zentrum Munich (Germany) and corresponding author of the study. “It shows that these non-pathogenic bacteria are not just passive residents but can actively manipulate human cells by injecting their proteins into our cells.”
Marianne Boes, PhD, Head of the Pediatric Immunology laboratory at UMC Utrecht (the Netherlands) adds: “This work shows that these injected bacteria-derived factors modulate the production of immune mediators by epithelial cells, that can directly influence intestinal health”.
To understand what these bacterial proteins do in human cells, the researchers mapped over a thousand interactions between bacterial effector proteins and human proteins, creating a large-scale interaction network. Their analyses showed that bacterial proteins preferentially target human pathways involved in immune regulation and metabolism. Further laboratory experiments confirmed that these proteins can modulate key immune signaling pathways, including NF-κB and cytokine responses. Cytokines are signaling molecules that help coordinate the immune system and prevent excessive reactions that can lead to autoimmune diseases. For example, inhibiting the activity of the cytokine Tumor Necrosis Factor (TNF) is a widely used treatment for Crohn’s disease, an autoimmune disease of the gut.
The researchers also found that genes encoding these bacterial effector proteins are enriched in the gut microbiomes of patients with Crohn’s disease. This suggests that direct protein delivery from gut bacteria to human cells may contribute to chronic intestinal inflammation, providing a potential mechanistic explanation for previously observed microbiome–disease links.
By identifying a previously unrecognized molecular layer between gut bacteria and the human immune system, the study advances our understanding of how the microbiome affects human cells, shifting research from correlation toward causation. It also raises intriguing questions, such as whether these injection systems evolved primarily for pathogenic purposes, or if they originally supported commensal coexistence and were later co-opted by pathogens.
Future research will aim to determine how individual bacterial effector–host interactions function in specific tissues and disease contexts, with the goal of translating these insights into more precise strategies for disease prevention and treatment.
Young V, Dohai B, Halder H, Fernandez-Macgregor J, van Heusden NS, Hitch TCA, Weller B, Hyden P, Saha D, Pieren DKJ, Rittchen S, Lambourne L, Maseko SB, Lin C-W, Tun YM, Bibus J, Pletschacher L, Boujeant M, Choteau SA, Bergogne L, Perrin J, Ober F, Schwehn P, Rothballer ST, Altmann M, Altmann S, Strobel A, Rothballer M, Tofaute M, Kotlarz D, Heinig M, Clavel T, Calderwood MA, Vidal M, Twizere J-C, Vincentelli R, Krappmann D, Boes M, Falter C, Rattei T, Brun C, Zanzoni A, Falter-Braun P. Effector–host interactome map links type III secretion systems in healthy gut microbiomes to immune modulation. Nature Microbiology, January 26, 2026.