A large international research by, amongst others, UMC Utrecht has uncovered how cancer is recognised and attacked by gamma delta T cells, a particular type of white blood cells. This gives hope for the future as it will help to make treatments more effective and better personalised. The results of the study have now been published in scientific journal Nature.
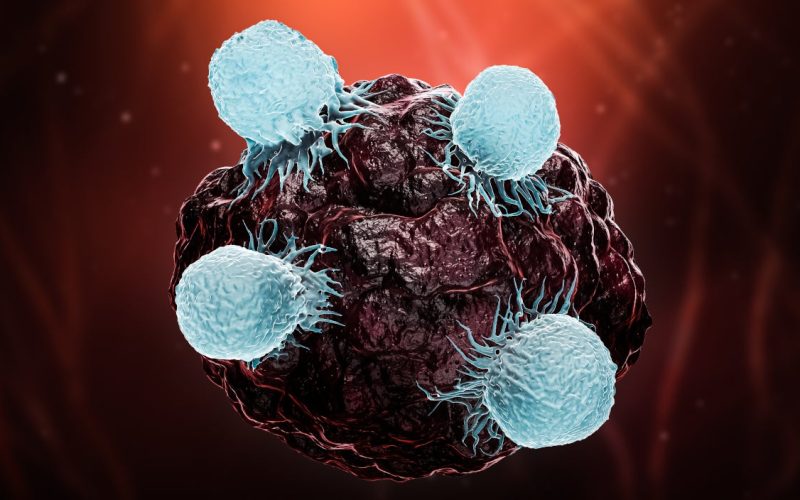
Virus, bacterium, cancer cell or other ‘invaders’: our body recognises them and battles them thanks to our army of T cells. These are a special kind of white blood cells that spring into action to clear away the danger. Today, this ingenious self-defence mechanism serves as the basis for designing many experimental immunotherapies.
A particular type of T cell, the gamma delta T cell, is an expert at recognising and targeting cancer cells. Exactly how this type of immune cell manages to do so was not yet known. This new research now provides the answer, using CRISPR technology, organoids and TEGs. For this joint effort, UMC Utrecht has collaborated with Gladstone Institutes and the University of California, San Francisco, among others.
Using the so-called ‘CRISPR technique’, the DNA of a cell can be cut up very specifically. As a result, the genetic properties of that cell can be manipulated. CRISPR allowed the researchers to disrupt thousands of genes in cancer cells to determine which modifications cause gamma delta T cells to attack cancer cells. By doing so, they could evaluate step by step, at the molecular level, how immune cells do their job.
The researchers also made use of ‘organoids‘. These are three-dimensional mini-organs or mini-tumours of about one millimetre in size, which are made from stem cells in a laboratory. Breast cancer and colon cancer organoids, which had been cultured in Utrecht, were used for this study.
Furthermore, they deployed ‘TEGs‘ for their research: a next generation of new, ‘living’ medicines containing genetically modified immune cells, which are being developed and tested in patients at UMC Utrecht.
How does a gamma delta T cell (or a TEG) know when it needs to spring into action? The researchers observed that gamma delta T cells start attacking a cell when butyrophilin levels in the cell start to skyrocket. Butyrophilin is a protein, which is also present in healthy cells. But in healthy cells, gamma delta T cells still keep quiet. The immune cells only start to attack when the quantity of butyrophilins starts to increase very rapidly, as is the case in a cancer cell.
What exactly causes this rise in butyrophilin levels? The researchers found that the quantity of butyrophilins grows when the cholesterol production in the cancer cell rapidly increases, or, in other words, when the cell starts to experience more ‘stress’. As soon as a cancer cell starts dividing, this typical stress reaction is triggered. Then, at lightning speed, more butyrophilins become active in the cell. This is the signal for the gamma delta T-cells to attack the invader, in this case the cancer cell.
Jürgen Kuball is professor of haematology, and Zsolt Sebestyen is associate professor, both at UMC Utrecht. They, together with their team, participated in this research.
Sebestyen: “With CRISPR, we removed the bits of gene that influence the ‘stress pathways’ of tumour organoids. And then we indeed saw confirmed that the stress response in a cell, via the increased butyrophilin levels, provides the key to influencing gamma delta T cells.”
This research is innovative because it means that scientists now exactly know at a molecular level how gamma delta T cells operate. This creates tremendous opportunities for future cancer treatment. One could think of therapies that influence butyrophilin levels, allowing the gamma delta T cells to act faster and fight cancer more effectively.
Kuball: “This study is an extraordinary collaboration between scientists doing basic (cell-oriented, ed.) and clinical-translational (patient-oriented, ed.) research. With its results, doctors and researchers can more specifically personalise immunotherapy with gamma delta T cells for patients. And, in addition, we may also be able to further develop new living medicines, such as TEGs, by using selective properties of gamma delta T cells.”