Advanced Therapy Medicinal Products or ATMPs are a novel class of interventions for human use that are based on genes, tissues, or cells. They offer groundbreaking new opportunities for the treatment of disease and injury.
ATMPs’ novel characteristics brings some unique challenges to bare. The novelty lays in their mechanism of action, live raw materials, intended function and manufacturing. They are often personalized products, reflecting or benefiting one or a few patients, and their production often requires two-directional transport of living cells or tissues. This asks a lot from supply chains but also from a privacy and regulatory standpoint.
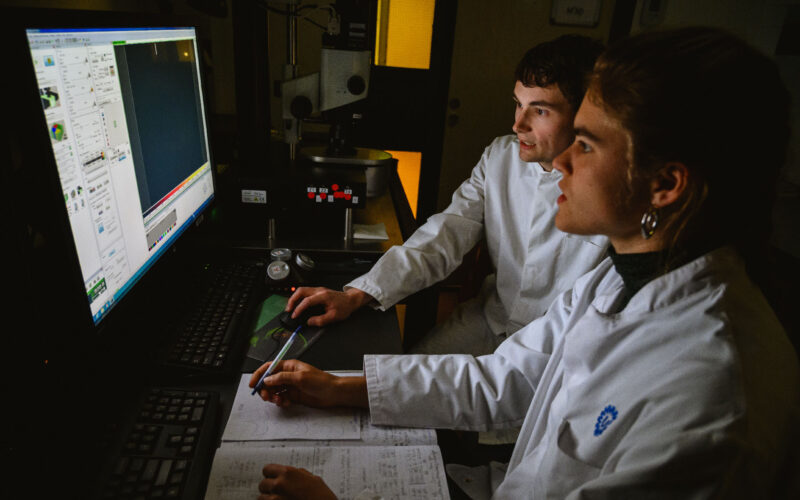
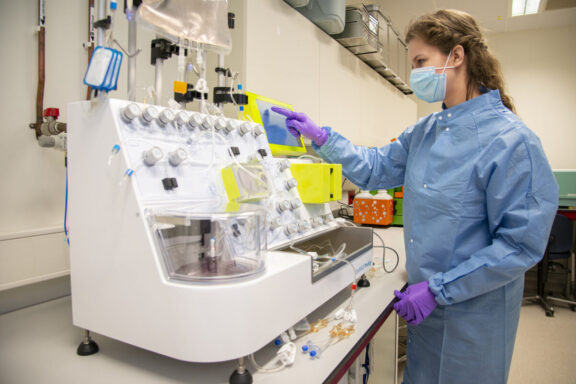
Utrecht is positioned in the middle of these development: we work on new regenerative therapies and ATMPs, we perform (early) Health Technology Assessment to inform product development and decision makers, and in ICAT (Innovation Center for Advanced Therapies) we have a pilot plant for the development of GMP and SMP standards. From this leading position within a leading country within ATMP development, we have a great vantage point.
According to the EMA, they can be classified into three main types:
From the perspective of health technology assessment (HTA), there are two main differences that set (regenerative) ATMPs apart from conventional therapies. First, the underlying technology and science is new, so especially the long-term effects are uncertain. Second, they combine this novelty with a different pricing mechanism. Currently, medicines are paid for as they are being used – and if the benefits wear off, it’s possible to stop the treatment and stop payment as well.
With ATMPs, especially gene therapies, the costs are mostly upfront. It is a high, one-time payment but it could have life-long effects. This means that if it indeed mitigates other healthcare costs for decades, a price of even a few million euros would be worth it. If it doesn’t live up to its promise, it may mean a significant loss, not only in quality of life but also financially. These are uncomfortable questions but at UMC Utrecht we do not shy away from them.
A challenge with ATMPs that is mostly noticed in the clinic is the hurdles that need to be overcome before these regenerative therapies and ATMPs can be applied to patients. Funding for the development of ATMPs is present from preclinical to clinical research, but there is a gap in knowledge and funding when it comes to the regulatory and translational aspects of therapies. In Utrecht, we have set up the ICAT to address this gap and help researchers with these steps.
The work of Roel Custers and his team is also exemplary in this regard. As a clinical researcher and orthopedic surgeon, he developed a new stem cell therapy for the treatment of damaged cartilage in the knee. After successfully guiding it through clinical trials, he now received a grant exclusively for the regulatory aspects, as well as HTA and IP-related issues. This project takes a year; a year during which patients can’t benefit from this treatment. Streamlining this process would be better for patients, doctors and institutions.
To overcome the regulatory challenges of ATMPs, Utrecht researchers were asked by ZonMw, in close collaboration with the Center for Future Affordable Sustainable Therapies development (FAST) to inform the Ministry of Health, Welfare and Sports to map the bottlenecks in ATMP regulation and admission and suggest solutions to them. In their report, the researchers praise the leading position of the Netherlands in regenerative medicine, but they also argue for more national coordination and harmonization of the rules, as well as patient engagement to ensure support.
Read the full reportA wide variety of diseases is caused by an error or mutation in our DNA. The consequences of these errors can vary from relatively mild symptoms in essentially any organ to a significantly reduced quality of life and life expectancy.
Stem cells possess the remarkable ability to self-renew and differentiate into specialized cells, offering hope for addressing various medical conditions.
Innovation Center for Advanced Therapies (ICAT) aims to improve and accelerate the translation of research into healthcare or clinical solutions.