Healthcare focuses more and more on personalized approaches. Since every person is different, 3D technologies play an increasingly important role in analyzing and mapping each patient’s unique needs. At UMC Utrecht, an innovative collaboration between 3D Lab and 3D Face Lab develops advanced technology such as 3D printers, scanners, prosthetics and implants to support both patients and doctors.
3D technologies open up many avenues in healthcare
Healthcare is moving towards truly personalized medicine. Regenerative medicine is a driving force behind that, with gene therapy or organoid-based diagnostics as examples. But personalized also means having a good view of individual patients, their anatomy, and their needs.
The unique collaboration between the 3D Lab and the 3D Face Lab develops these technologies forward with multiple applications. First of all, they utilize 3D scans and models to prepare for and guide surgery. Second, they use 3D technology to create the best fitting implants. And finally, the three-dimensional aspect helps to advance implants towards more regenerative, smart implants. This article will provide an overview of these three routes.
‘With these 3D images, we can develop detailed surgical plans, optimize approaches, and simulate surgical outcomes before the intervention takes place.’
Using 3D imaging to prepare for surgeries…
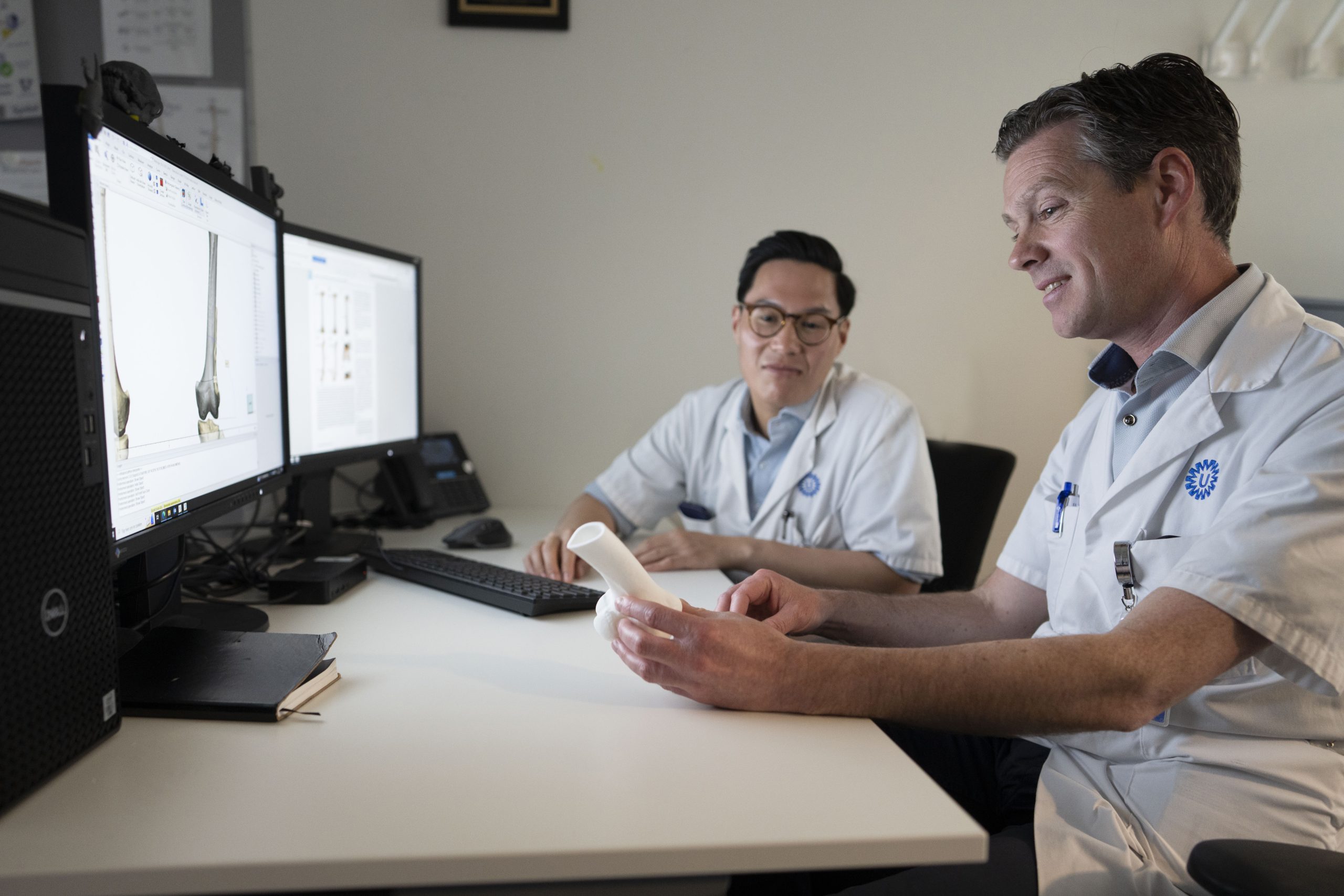
Implants, prosthetics, surgical guides and other customized treatments for individual patients rely on high-quality 3D visualization. Therefore, the work of the 3D Lab and 3D Face Lab starts with excellent scans, made with CT or MRI. ‘With these 3D images, we can develop detailed surgical plans, optimize approaches, and simulate surgical outcomes before the intervention takes place,’ explains Joël Kortes, trainee Qualified medical engineer and coordinator of the 3D Face Lab.
The 3D Face Lab is located next to the 3D Lab in the UMC Utrecht and is a specialized technical laboratory for the Department of Oral, and Maxillofacial Surgery, and Special Dental Care. This lab performs technical and digital work on behalf of dentists for patients with care needs related to the mouth, jaws, face, and related structures.
… and for intraoperative guidance
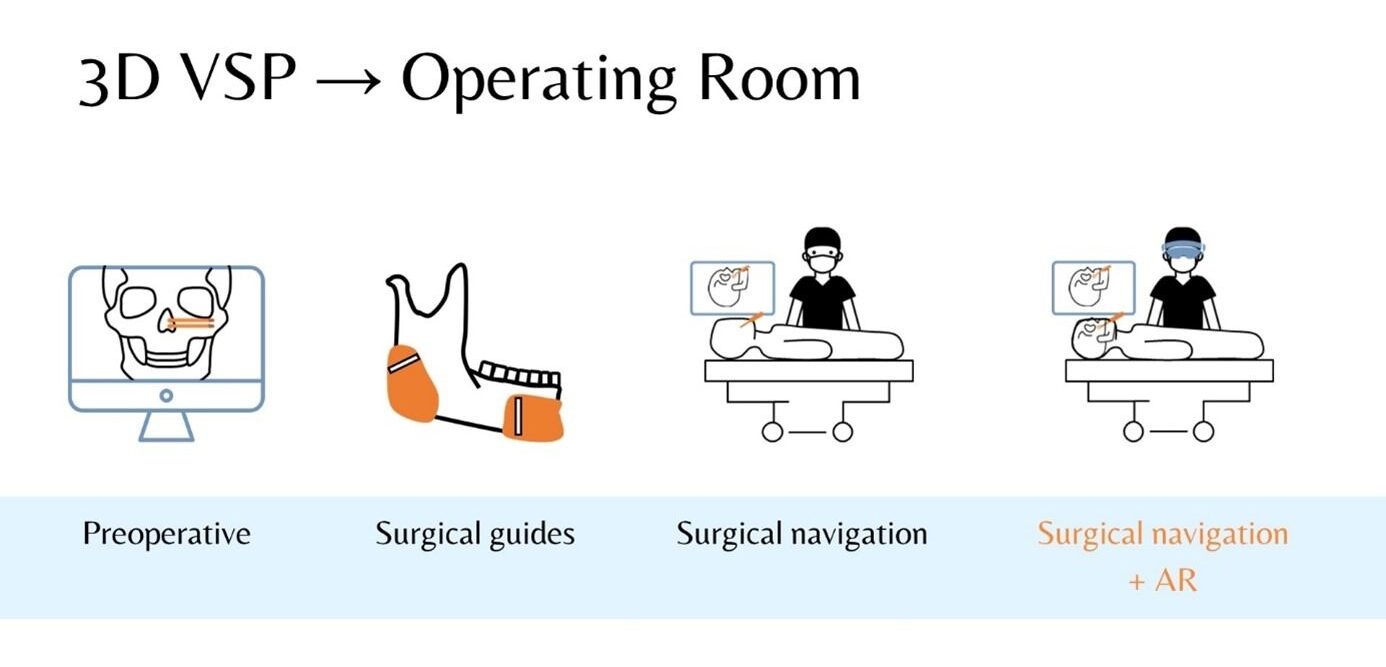
‘We can transfer these digital surgical plans to the operating room using surgical navigation systems and computer-aided techniques,’ Kortes continues. ‘For example, 3D-printed surgical guides and surgical navigation methods help surgeons accurately track where their instruments and the patient are during surgery, using preoperative images as a reference.’
These virtual surgical planning (VSP) methods are beneficial in multiple ways, explains Joël: ‘By supporting the surgeons in complex operations, the treatment becomes more predictable, more accurate, and safer for the patient.’

‘We developed a 3D-printed shelf implant to enlarge the hip socket. These implants provide an alternative to pelvic osteotomies, a surgical intervention.’
Augmented reality can augment a surgery
The surgical navigation systems can be used in combination with augmented or extended reality glasses. Kortes: ‘Augmented reality (AR) is a technology that enhances the real world by overlaying virtual objects on it. Unlike virtual reality (VR), the real world remains visible.’ Extended reality (XR, the umbrella term for AR, VR and Mixed Reality (MR)) also promotes efficiency and accuracy during surgical procedures. Kortes explains: ‘XR offers an immersive experience that integrates all kinds of information into a single view, allowing healthcare providers to switch between different systems without taking their eyes off the patient.’
Case: 3D-printed implants for hip dysplasia
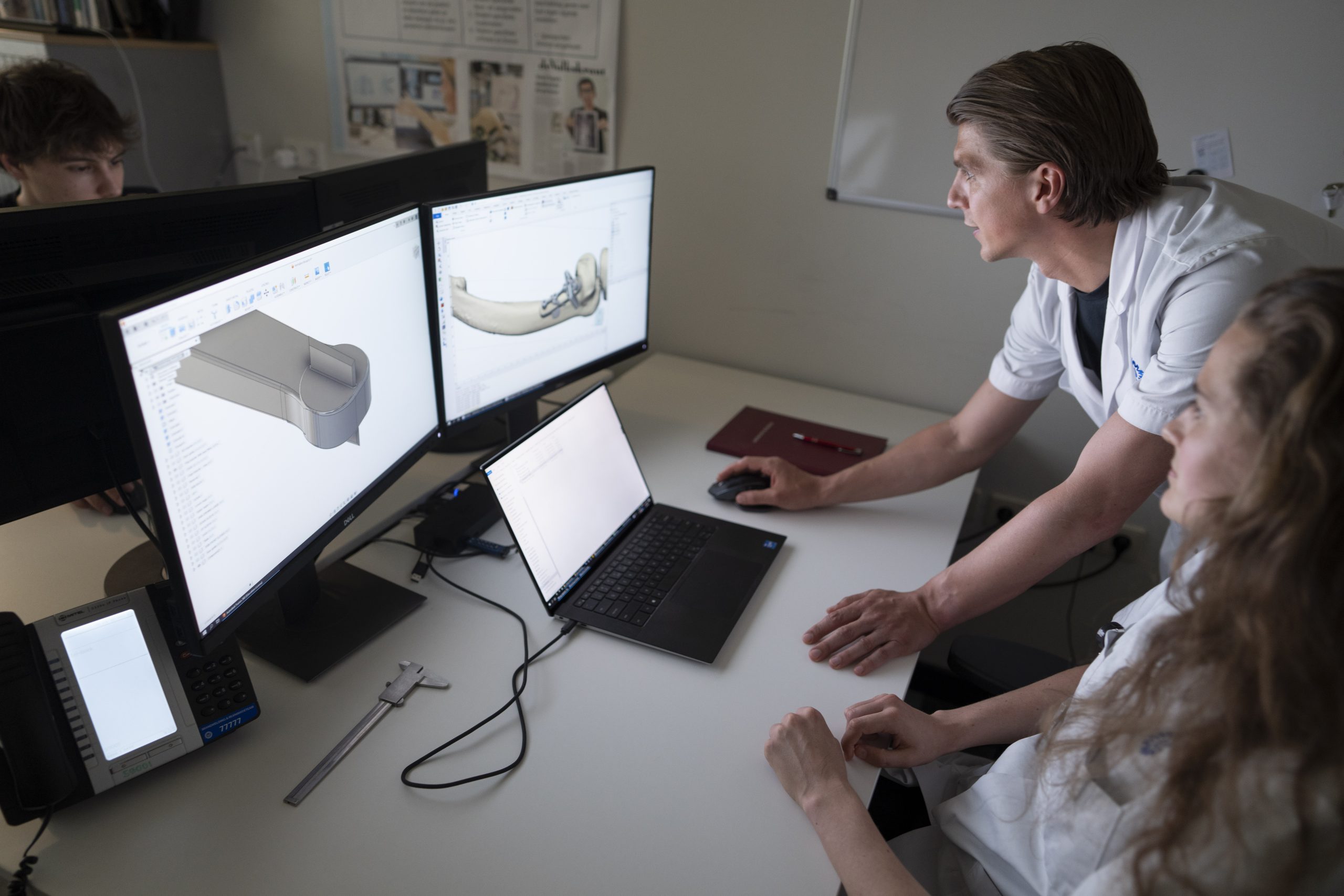
Another use for 3D technology and imaging is the development of personalized implants. The 3D Lab of the UMC Utrecht is involved in research into the three-dimensional nature of hip dysplasia.

Joëll Magré, biomedical engineer and coordinator of the 3D Lab, explains: ‘Hip dysplasia is an anomaly where the hip joint is not properly developed. The hip socket is too shallow, allowing the femoral head to slip partially or completely out of the socket. Additionally, the shallow hip socket increases pressure on the joint, which could lead to the early development of osteoarthrosis.’ Often, surgical intervention is needed.
A better implant helps forego bone surgery
The 3D Lab researches innovative treatments for this anomaly using 3D-printed implants. ‘We developed a 3D-printed shelf implant to enlarge the hip socket,’ Magré states. ‘These implants provide an alternative to pelvic osteotomies, a surgical intervention which changes the shape or position of the pelvic bones so that the hip socket better covers and supports the femoral head.’
Designing implants from the One Health perspective
Hip dysplasia is something that humans suffer from, but also other animals like dogs. UMC Utrecht therefore works closely with the Faculty of Veterinary Medicine of Utrecht University, and their veterinary patients.
‘We are now selecting a second group of dogs with hip dysplasia that will receive a custom-made 3D-printed implant,’ Magré explains. ‘Simultaneously, we are researching the morphological differences and 3D anatomy of hip dysplasia in humans to develop a 3D-printed shelf implant for human application.’

Smart implants: the next step in regenerative implants
What the hip dysplasia implants show, is that the 3D Lab has extensive expertise designing specific metal implants, tailored to meet the unique needs of each patient for varying pathologies. Currently, these implants are designed to be bio-inert, meaning that they do not induce a biological reaction between the implant and the recipient. But the 3D Lab is also working on a new kind of implant – a regenerative implant. One example of an innovative solution that makes implants ‘smart’ is 3D-printed porous structures that allow bone ingrowth. This increases the implant stability and longevity.
A smart implant to help the body
However, the 3D Lab specialists aim for further improvements. ‘We need smarter implants that can withstand the lifecycle of a patient,’ says Chien Nguyen, technical physician and also coordinator of the 3D Lab. ‘In the search for smarter and more durable implants, we focus on two strategies that use human biology to improve the implant: mechanical and biological factors. We try to harness these factors to trigger tissue integration and adaptation to the implant.’
‘We need smarter implants that can withstand the lifecycle of a patient.’
Using mechanical factors in implant design
The first of these novel implant strategies uses mechanical forces. ‘What is fascinating about human bones,’ Nguyen begins, ‘is that they are capable of monitoring mechanical load, and re- or degenerate bone tissue depending on the need of each bone.’ The 3D Lab researches smart metal implants that are capable of applying mechanical stress to bone tissue. ‘We learned that loading of a bone is crucial to keep the structures strong and to induce regeneration, so we consider this in our implant designs.’

Developing a smart metal implant for hip replacements
The first application of a smart metal implant was studied in hip replacement, where current implants can lead to large bone defects in the hip socket. ‘These personalized 3D printed implants remove the necessary mechanical stress on this bone tissue, causing it to degenerate,’ Nguyen explains. To solve this issue, the team uses advanced 3D printing technology. ‘We engineered a deformable titanium mesh structure that is capable of dynamically adjusting its morphology under pressure. This adaptability enables the implant to effectively apply mechanical stress to hip socket defects. The result is optimal support and stability, and, hopefully, a trigger for the bone tissue to regenerate.’

Using biological factors in implant design
The second strategy goes further than inducing bone regeneration with a mechanical stimulus. This research is in collaboration with the group of Jos Malda, professor of Biofabrication in Translational Regenerative Medicine. Nguyen: ‘This approach stimulates bone growth using biological factors, ultimately aiming at the total resorption of the implant. To achieve this, we print ceramic materials as bone substitutes.’ In contrast to current implants, these materials are bioactive, meaning that the implant induces a biological reaction between the implant and the recipient.
Working towards implants with bone-generating properties
‘Among the bioactive ceramic materials that have been used for bone tissue engineering, magnesium strontium phosphate has gained particular interest,’ Nguyen begins. ‘Magnesium phosphate is soluble under physiological conditions, and the strontium ions promote the differentiation of mesenchymal stromal cells (MSCs) into bone-producing cells.’ The group of prof. Malda also came up with a solution for the ceramic scaffolds’ brittle characteristics, which makes them prone to fracture, making the implants usable for the 3D Lab. ‘By adding polycaprolactone (PCL), a synthetic polymer, we were able to 3D-print mechanically stable implants with the same bone-producing properties.’
Enhancing implant integration
Finally, it may be possible to seed the ceramic scaffold with a bioactive product such as bone marrow concentrate, Nguyen explains. ‘Presurgical seeding of the implant could accelerate the integration of the implant with the native bone tissue of the patient, resulting in a more durable implant with a potential lifespan that is the same as the patient’s.
Steps towards integration and regeneration
In the near future, 3D technologies as the ones discussed will combine and augment each other. A patient might benefit from a smart implant that is inserted by a surgeon aided by 3D models in AR. A bit further away, smart implants may become more and more based on the patient’s own cells and tissues. This is where the work of the 3D Lab merges into biofabrication. And even a fully printed organ or implant will still rely on representative 3D models of the patient, so 3D technology is here to stay.
