A lot of heart diseases result in the loss of functional heart tissue, leading to further complications and loss of quality of life. Biofabrication, the printing of cells into (parts of) functional organs, is a promising technology to repair the heart after an event. At UMC Utrecht, the Experimental Cardiology group is exploring how biofabrication can repair the damaged heart.
Losing tissue after a heart attack
During a heart attack, when an artery supplying the heart muscle is blocked, up to a billion cells suffer from oxygen starvation. This means that part of the heart muscle dies, forming scar tissue and weakening the heart’s function. To compensate for this loss, the rest of the heart muscle must work harder. However, this means that the remaining heart muscle slowly deteriorates, leading to heart failure.
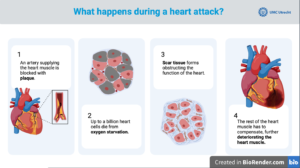
Infographic: What happens during a heart attack?
From LVAD to Bio-VAD
Patients with heart failure currently rely on a Left Ventricle Assisting Device (LVAD), an artificial device to help their heart pump while they wait for a heart transplant. LVADs have increased life expectancy, but it remains an external artificial device. This means that patients living with an LVAD need to stay in range of a power source, cannot swim and need to carefully manage the device’s stoma to reduce risk of infections.
Alain van Mil and his colleagues of the Experimental Cardiology group at UMC Utrecht are working on finding a better solution in regenerative medicine. As part of the BRAVE consortium, they are developing a so-called Bio-VAD. This is a biological VAD, using a patient’s own cells to regenerate their heart muscle. A Bio-VAD would solve the issues of the current standard of care, but it’s a multifaceted challenge to develop one. Not only does it require the right type of cell and in sufficient numbers, it demands also that the cells function in concert with the rest of the moving, beating heart.
“We had to work hard on optimizing culturing conditions to facilitate the differentiation of cells, and to develop a culturing method to be able to obtain the billions of cardiomyocytes needed for a clinically relevant intervention.”
Culturing enough heart cells
Since the development of iPSC (induced pluripotent stem cell) technology, researchers can culture cardiomyocytes from the patient’s own cells. ‘These cells are perfect for implantation,’ says Van Mil, ‘but we had to work hard on optimizing culturing conditions to facilitate the differentiation of cells, and to develop a culturing method to be able to obtain the billions of cardiomyocytes needed for a clinically relevant intervention.’
Getting heart cells to align and organize
Heart muscle tissue is highly organized to facilitate all cells beating in synchrony. However, when iPSC-derived cardiomyocytes are simply mixed with a hydrogel to form a patch, the cells remain in an unorganized tissue structure. This means the signal transduction and contraction forces are not aligned, which are critical to increase pump function.
To overcome this, the Experimental Cardiology group had the idea to incorporate a scaffold that would mimic the highly organized tissue fiber structure seen in the adult heart, allowing the cells to align. Van Mil: ‘To achieve this, we worked in close collaboration with the Biofabrication team led by Prof. Jos Malda, which had developed Melt Electro writing or MEW technology. This technology allowed us to create structures like the heart’s extracellular matrix at a high resolution.’
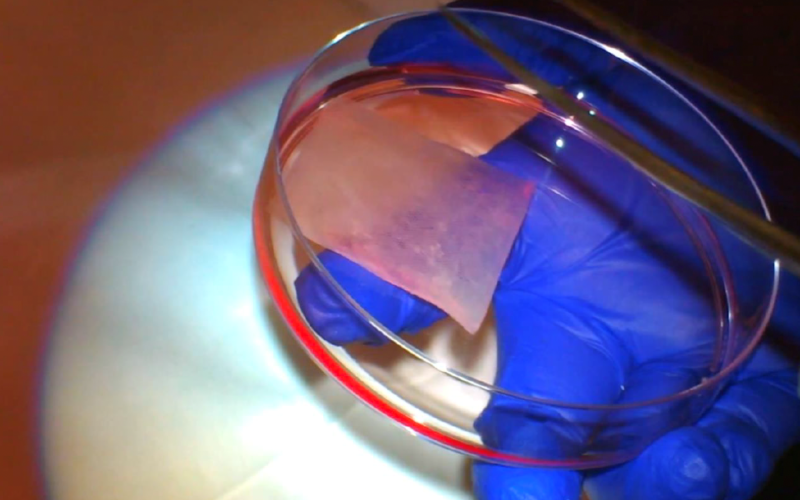
Experimenting with scaffolds
The team started with a simple grid pattern scaffold to which the hydrogel with cells was added. ‘While the cells aligned to the structure, the stiff, rectangular pattern did not allow for the patch to stretch with the beating of the heart and it tore,’ Van Mil observes. The group went back to the drawing board and looked at the heart muscle’s structure. They found that the extracellular matrix of the human heart is organized in a beehive-like pattern comprising of hexagonal structures, which led to the next iteration of the patch.
A hexagon-shaped box
When the group printed the scaffold using a hexagonal pattern, it was able to follow the beating of the heart without tearing. ‘When we added the gel with cardiomyocytes, they followed the structure of the printed fibers and the iPSC-cardiomyocytes were found to mature much better,’ Van Mil reflects. ‘The next challenge is to make them of a clinically relevant thickness.’
Patch thickness should match the human ventricle
The muscle wall of human ventricles is 5-7mm thick. However, MEW printing of these complex hexagonal microarchitectures, on the other hand, can only reach up to 1mm thickness at the required resolution. Therefore, the group experimented with stacking multiple patches. Van Mil explains how they also optimized this step: ‘3D imaging shows that the heart not only contracts but also twists and untwists with each beat. We therefore decided to stack patches at slightly different orientations. These stacked patches were able to function very well.’
“3D imaging shows that the heart not only contracts but also twists and untwists with each beat. We therefore decided to stack patches at slightly different orientations. These stacked patches were able to function very well.”
How to attach the patch to the heart – and where
For a patch to work, it needs to remain securely attached to the patient’s heart while allowing the cells to function. Van Mil: ‘The first trials with tissue glue showed that the glue blocked the communication between the heart and the patch cells, hindering its function. Therefore, we now fasten it to the heart with sutures that have a bit of stretch.’ Imaging revealed that this technique results in good integration with the surrounding tissue.
‘While it might seem logical to place the patch on the scar tissue,’ Van Mil explains, ‘this tissue is not functional and only contains a very small population of cardiomyocytes. This does not allow proper integration of the patch. It is therefore better to design a patch that can cover both healthy tissue and the scar, to allow coupling with the still functional areas and better support the beating of the heart.’
“We are now at a stage where we can create a cell-patch that can be added to the exterior of the heart. But we need the cells to be able to beat with the heart muscle. To achieve this, we are working on deciphering the mechanisms that control cardiomyocyte migration, which could be employed to enhance patch integration with the host tissue.”
Working towards added value for each patient
In a clinical setting, the cardiac patch would need to be available for each patient in a timely manner, so the team is developing methods to cryopreserve cardiac patches, aiding in off-the-shelf availability, ultimately increasing their clinical applicability.
‘At the same time,’ Van Mil says, ‘infarctions can differ in location and severity, so a personalized approach is also necessary. To achieve this, each patient could be evaluated using an MRI of the heart, and researchers could design a personalized patch of the needed shape and size.’
Arming the lab with better technology
The next step in the development of complex patches has been the acquisition of an advanced robotic arm that connects to the MEW printer. ‘This arm allows for more degrees of freedom in printing, which in turn makes it possible to print more complex patches, taking into account the specific geometries of a patient’s heart and infarct. It’s exciting to see where this will take us,’ Van Mil concludes.