During the COVID-19 pandemic – especially during the first wave of infections- a large number of people infected with the SARS-CoV-2 virus reported a sudden loss of smell. Dutch investigators quickly set up a series of studies on diagnosis, pathophysiology, epidemiology, clinical course and treatment of COVID-19-induced loss of smell. The PhD thesis by Emma Schepens (UMC Utrecht) provides some interesting and valuable insights on this unexpected clinical finding.
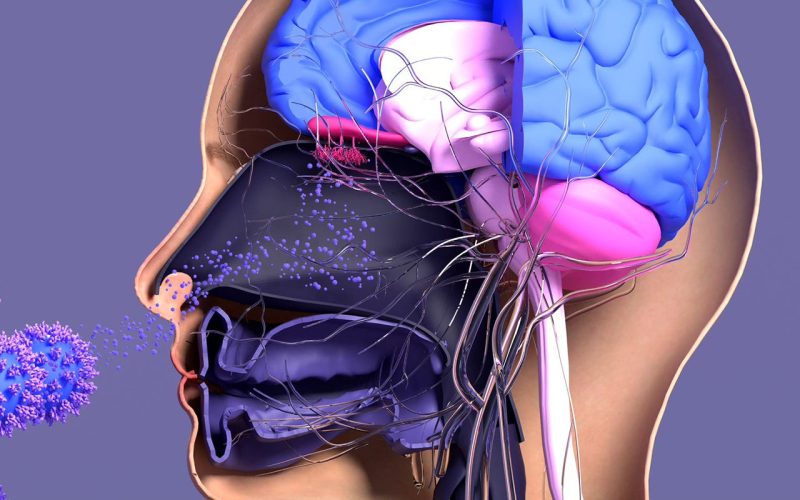
The sense of smell is often underappreciated and profoundly impacts our daily lives by influencing our well-being, eating behaviors, social interactions, emotions, and memories. The COVID-19 pandemic starkly highlighted this when countless people reported a sudden loss of smell and taste following infection with the SARS-CoV-2 virus. Emma Schepens, a PhD candidate in the Department of Otorhinolaryngology at UMC Utrecht, embarked on a pioneering journey to explore the diagnosis, treatment, and clinical progression of COVID-19-related smell loss.
Persistent smell loss post-COVID-19 is thought to result from an inflammatory response, suggesting that corticosteroids like prednisolone might offer relief. To test this hypothesis, Schepens and her team conducted the COCOS (COrticosteroids for COvid-19 induced loss of Smell) study, a randomized controlled double-blind multicenter study. The results, however, were disappointing: the study, involving 115 patients, revealed no significant difference in recovery between those treated with prednisolone and those given a placebo.
Schepens explained, “After treatment, there was no greater improvement in the sense of smell in patients who were on prednisolone (40 mg/day for 10 days, starting at least four weeks after infection) compared to those who received a placebo.” Despite this, there was a silver lining: in an extension study of the COCOS trial both groups exhibited continued improvement in their sense of smell over time, even up to a year post-infection, though the rate of recovery diminished with time.
One noteworthy finding from Schepens’ research was the positive impact of smell training. A 12-week regimen of olfactory exercises suggested favorable effects on restoring the sense of smell in COVID-19 patients. This discovery opens new avenues for non-pharmacological interventions to help those suffering from long-term loos of smell.
Accurate diagnosis of smell loss is crucial for effective treatment. Schepens and her colleagues evaluated the Sniffin’ Sticks Test (SST-12) for its efficacy in detecting COVID-19-induced smell loss. Their research confirmed the SST-12 as a valuable and quick screening tool for clinical practice. Additionally, comparative studies indicated that COVID-19 patients experienced more frequent and severe smell loss than those with non-COVID-19-related smell disorders, though the latter group faced longer-lasting symptoms.
Olfactory disorders emerged as a common early symptom of COVID-19, affecting approximately two out of every three patients. While most individuals regained their sense of smell within four weeks, up to 46 percent continued to experience impaired olfaction after six months, and between 20 to 60 percent remained affected after a year. The variability in these statistics is due to differing methods of olfactory function assessment and inconsistent follow-up.
Emma Schepens’ research offers critical insights into the diagnosis and potential treatments for COVID-19-related smell loss. While prednisolone may not be the answer, the potential of smell training and accurate diagnostic tools like the SST-12 provide hope. As the medical community continues to navigate the long-term impacts of COVID-19, Schepens’ work underscores the importance of ongoing research and innovation in addressing the nuanced and often overlooked consequences of this global pandemic.
Emma Schepens, MD (1993, Laren) defended her PhD thesis on May 23, 2024 at Utrecht University. The title of her thesis was “Scent & Sensibility – A journey towards recovery in COVID-19 induced olfactory disorders”. Supervisors were Prof. Robert Stokroos, MD PhD (Department of Otorhinolaryngology, UMC Utrecht) and Sanne Boesveldt, PhD (Wageningen University & Research, Wageningen). Co-supervisors were Digna Kamalski, MD PhD and Inge Stegeman, PhD (both Department of Otorhinolaryngology, UMC Utrecht).