The incidence of pneumonia due to infection with Staphylococcus aureus at the intensive care may be higher than previously thought. Future interventions to prevent this condition should therefore focus on patients colonized with S. aureus, says Fleur Paling in her PhD research.
The Staphylococcus aureus bacterium is both a human commensal and an opportunistic pathogen. Approximately 25-30 percent of healthy people carry the bacterium on their skin or in their respiratory tract. At the same time, S. aureus is a true pathogen in disguise and has the potential to quickly develop into a serious or even life-threatening infection. Carriers of S. aureus are known to have an increased risk of acquiring an S. aureus infection, especially in the critically ill, after surgery, when on renal dialysis and in people with a compromised immune system.
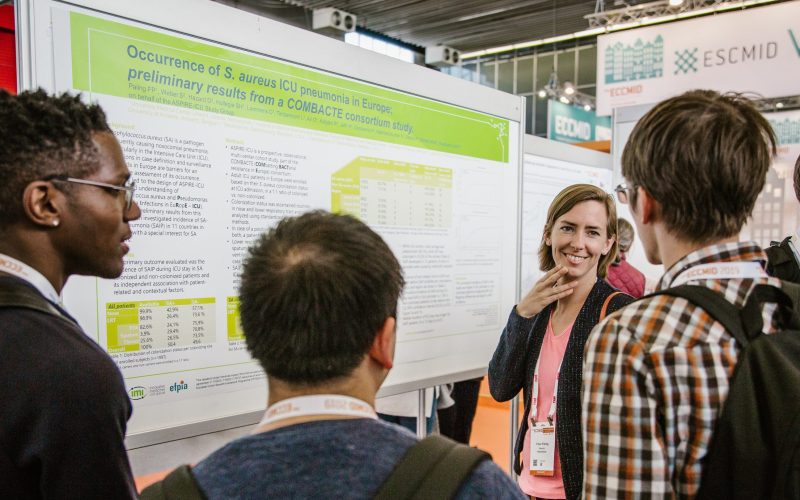
To date, associations between S. aureus carriage and the development of S. aureus intensive care-acquired pneumonia (SAIP) have not been quantified accurately, and interpretation of available data is hampered due to variations in definitions. In order to get a deeper insight in SAIP, Fleur Paling (Julius Center for Health Sciences and Primary Care, UMC Utrecht) and colleagues started in 2015 a study (ASPIRE-ICU) to determine the incidence of SAIP in Europe, and which factors are associated with the risk of SAIP. The key findings of this study have just been published in JAMA Network Open.
The study consisted of 1.997 patients, of which 1.933 were used for this analysis. 950 of these were S. aureus carriers at ICU admission. The overall incidence of SAIP at the ICU was 4.9 events per 1000 patient-days. There was a marked difference between colonized and non-colonized patients: SAIP incidences were 11.7 events per 1000 patient-days for S. aureus–colonized patients, compared to just 2.9 events per 1000 patient-days for non-colonized patients. Further analysis revealed that S. aureus colonization status remained the only factor that was independently associated with SAIP (hazard ratio 3.6; 95 percent CI 2.2-6.0; P<0.001).
Fleur Paling concludes: “Our findings suggest that the incidence of pneumonia at the ICU due to S. aureus infection may be higher than initially perceived, and future interventions to prevent pneumonia at the ICU should focus on patients colonized with S. aureus.”
ASPIRE-ICU (which stands for Advanced understanding of Staphylococcus aureus and Pseudomonas aeruginosa Infections in EuRopE – Intensive Care Units) is a prospective, observational, multicenter, epidemiological cohort study that ran from 2015-2018. The study was nested within routine surveillance among ICU patients and aimed at the advanced understanding of S. aureus and Pseudomonas aeruginosa infections in Europe. The study was conducted in ICUs of 30 hospitals in 11 European countries. ASPIRE-ICU is part of the IMI-sponsored public-private COMBACTE project.
Fleur Paling (1985, Groningen) will defend her PhD thesis on October 20, 2020 at Utrecht University. The title of her thesis is “The role of carriage in the development of healthcare-associated infections with S. aureus and P. aeruginosa”. Supervisors are prof. dr. Jan Kluytmans and prof. dr. Marc Bonten (both Julius Center for Health Sciences and Primary Care, UMC Utrecht). Fleur Paling is finalizing her training to become a general practitioner by the end of 2020.