Staphylococcal protein A is an important immune evasion factor and potential vaccine antigen of the bacterium S. aureus. The protein is likely one of the main contributing factors for the poor efficacy of the antibody-dependent immune response against S. aureus. Ana Rita Cruz at UMC Utrecht concludes in her PhD thesis that understanding how SpA blocks IgG effector functions may help to gain insight for the development of successful anti-S. aureus therapies that can be used as alternatives to antibiotics.
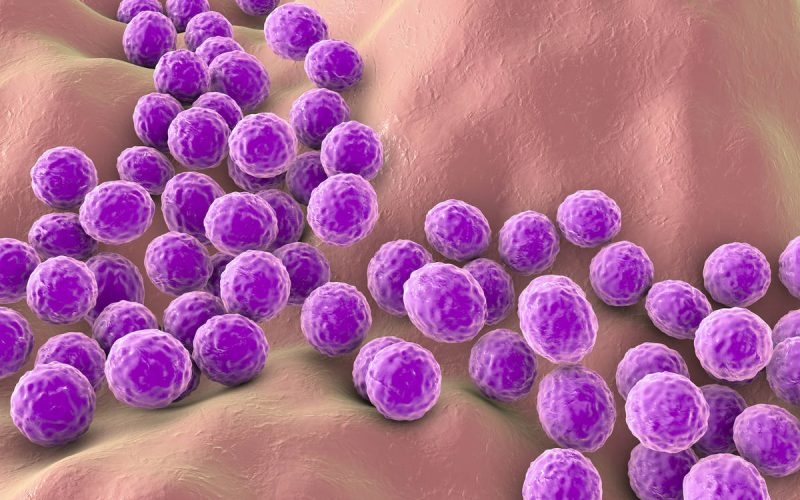
Antibiotic resistance is a major problem for public health. Staphylococcus aureus, a well-known multi-drug resistant bacterium or simply as “super bug”, is one of the pathogens for which new antibiotics and other therapeutic options are urgently needed. S. aureus can cause mild to life-threatening diseases that include skin and soft tissue infections, pneumonia, infective endocarditis, osteomyelitis and sepsis. Although our immune defenses protect our body from invading bacteria, some pathogens – including S. aureus – have evolved strategies to evade the host immune system.
One particularly important immune evasion factor of S. aureus is staphylococcal protein A (SpA). SpA binds to the constant region of antibodies to prevent phagocytic cells from recognizing S. aureus. Antibodies have a variable and a constant region. The variable region can recognize antigens that are secreted by the bacteria, or that are exposed on their surfaces. When antibodies bind to surface antigens via their variable region, their constant region can trigger bacterial clearance by inducing complement activation and by interacting directly with immune cells, like neutrophils. Decoration of the bacteria with antibodies and complement proteins is essential for their recognition by phagocytic cells. Upon recognition, these cells engulf and kill the bacteria intracellularly. In this thesis, PhD candidate Ana Rita Cruz (Department of Medical Microbiology, UMC Utrecht and GSK, Siena, Italy) focused on understanding how SpA, by binding to the constant region of antibodies, interferes with antibody- and complement-mediated phagocytosis of S. aureus.
Ana Rita Cruz and colleagues unveiled how SpA, by binding to the constant region of antibodies, prevents phagocytic killing of S. aureus. For optimal complement activation, IgG molecules (the most abundant antibody type in serum), should organize into groups of six antibodies, to form IgG hexamers. Bacteria decoration with complement proteins strongly enhances effective phagocytosis and killing of S. aureus. The investigators showed that SpA inhibits antibody-dependent complement activation by interfering with the formation of IgG hexamers. Additionally, they demonstrate that SpA inhibits the interaction of antibodies with Fc gamma receptors and the neonatal Fc receptor. The interaction of these receptors with antibody-decorated bacteria is important for effective phagocytosis.
Ana Rita Cruz summarizes the significance of her findings: “SpA is an important immune evasion factor and potential vaccine antigen of S. aureus. SpA is likely one of the main contributing factors for the poor efficacy of the antibody-dependent immune response against S. aureus. Thus, understanding how SpA blocks IgG effector functions may help to gain insight for the development of successful anti-S. aureus therapies that can be used as alternatives to antibiotics.”
Ana Rita Cruz (1992, Coimbra, Portugal) defended her PhD thesis on January 13, 2022 at Utrecht University. The title of her thesis is “How staphylococcal protein A blocks IgG effector functions”. Supervisors were prof. dr. Jos van Strijp and prof. dr. Suzan Rooijakkers (both Department of Medical Microbiology, UMC Utrecht). Co-supervisor was dr. Andrea Manetti (GSK, Siena, Italy). This PhD project was part of DISSection and was funded as a H2020 Marie Curie ITN project.