Brain organoids are three-dimensional clusters of cells that mimic the human brain. They can be grown (in the laboratory) from skin cells of healthy people or patients. When Astrid van der Geest started with her PhD research six years ago, this technique was still relatively new. It enabled Astrid to compare brain development in ALS patients at the cellular level with that of healthy individuals. Now her dissertation is complete, and she will defend it on Tuesday, November 4, at the Academiegebouw in Utrecht. Thanks to her research, we now have much more knowledge about the properties of early brain development in people with ALS and how these differ from healthy brains.
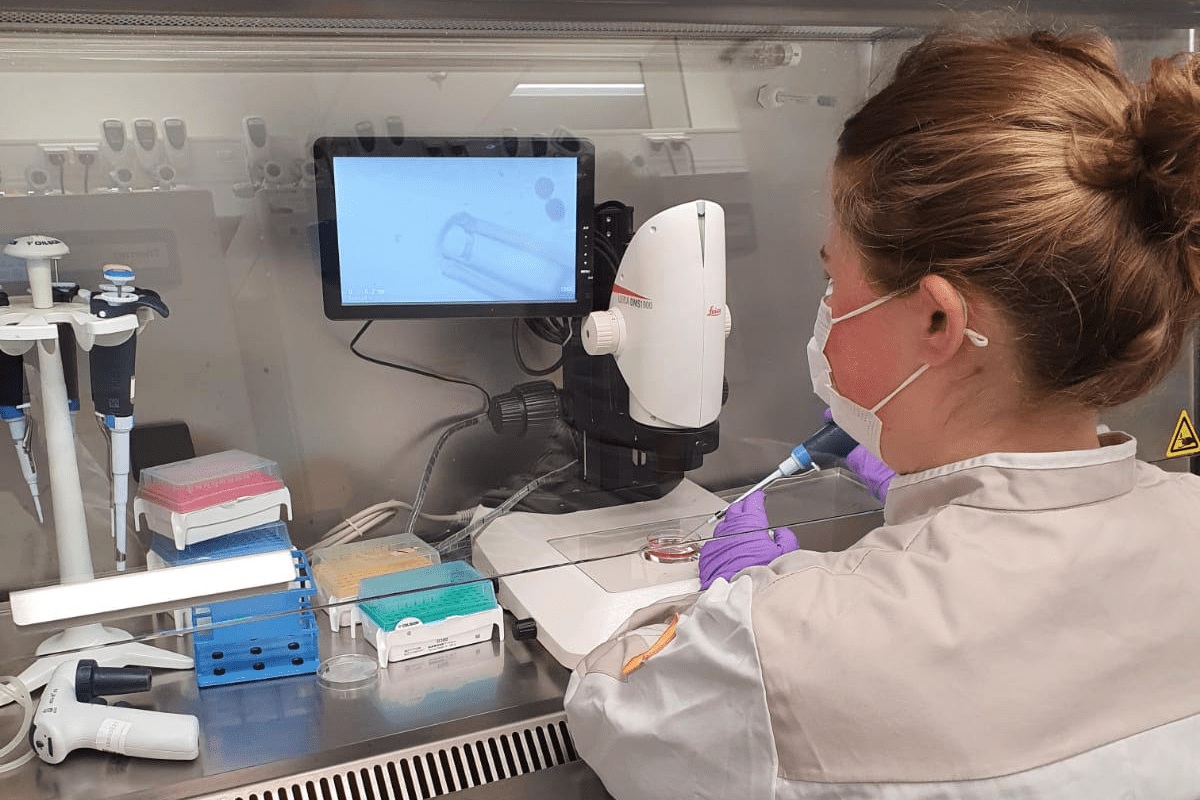
Astrid explains how her research started six years ago: “When you try to trace the origin of ALS in an individual, you run into the problem that brains are not easy to study, you can’t just take them out of the body. In the years before my PhD, new techniques became available that allowed us to develop a model that strongly resembles the brain: brain organoids.” When creating brain organoids, (healthy) human skin cells are used. These cells are treated in the lab so that they acquire a stem cell identity.
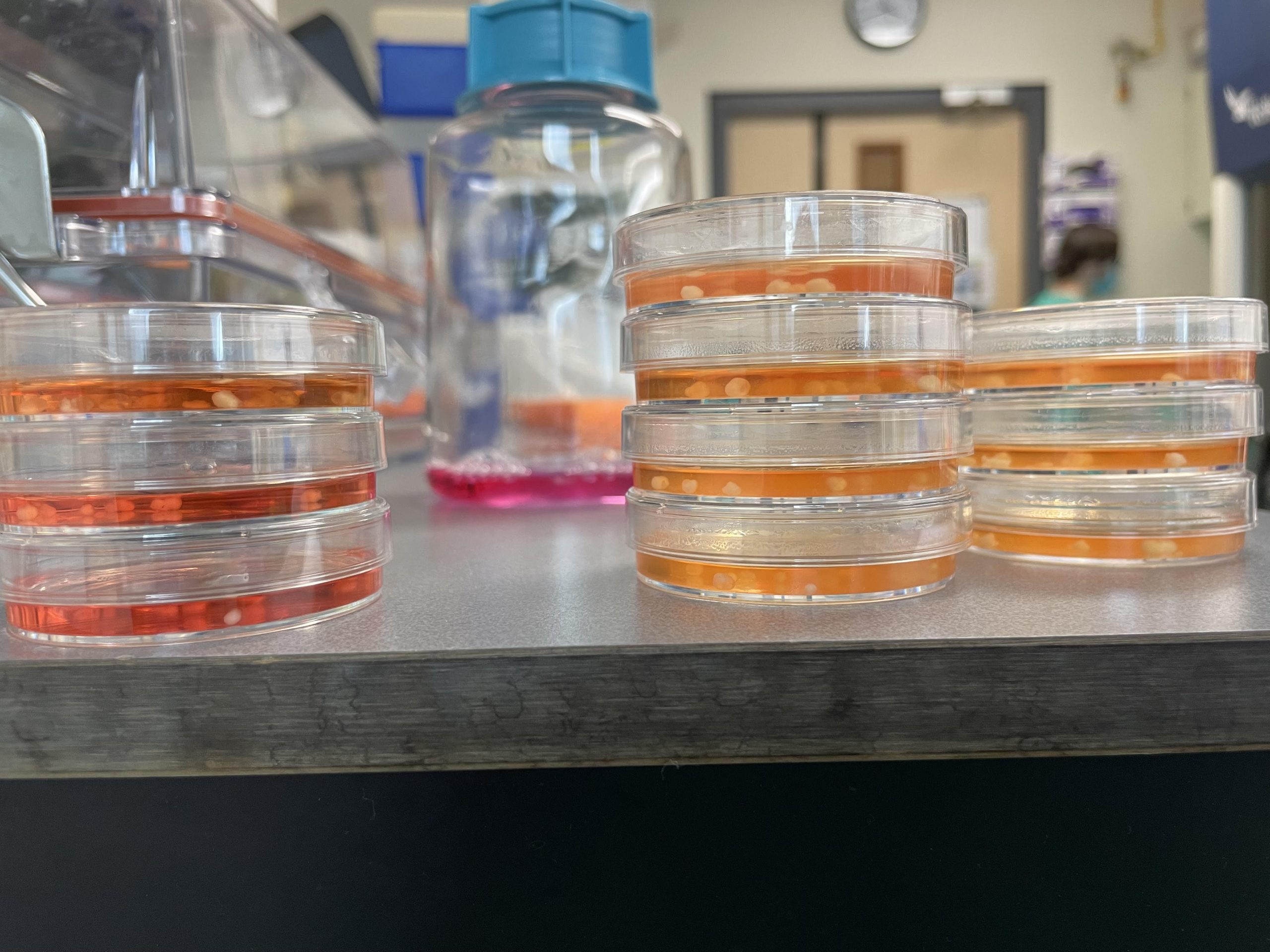
Organoids in petri dishes.
“A stem cell can be compared to an embryo-like cell, it can still develop in many different directions. By adding various substances, the cells can develop into, for example, a limb or skin. If we let the stem cells develop on their own, with little to no signaling substances added, they gradually form a brain.”
Astrid illustrates the size of such a brain organoid with her hand. “It’s a tissue cluster consisting of millions of cells that grows to just a few millimeters in size. You can actually see it with the naked eye.” That little cluster of cells grows and slowly matures. Because you can easily observe the brain cells, you can also clearly compare how these cells develop in organoids made from ALS patients versus healthy individuals.
Astrid explains that she mainly observed what happens when organoids are allowed to develop. “We soon noticed abnormalities in the brain organoids from ALS patients: they initially grew much faster. After that, the growth stagnated and reached a plateau. The healthy brain organoids, on the other hand, grew more slowly but more steadily and for a longer period.” These results resemble what was already known from earlier MRI studies (for example, in the research by Henk-Jan Westeneng): the outer layer of the brain (the cortex) in ALS patients is thinner, even years before symptoms appear.
“We were actually surprised at how quickly we saw results and differences. Then we realized that the brain organoid lies completely exposed, with only some nutrients in a petri dish; there’s no body to remove waste products. In short, it’s a pressure cooker for problems.”
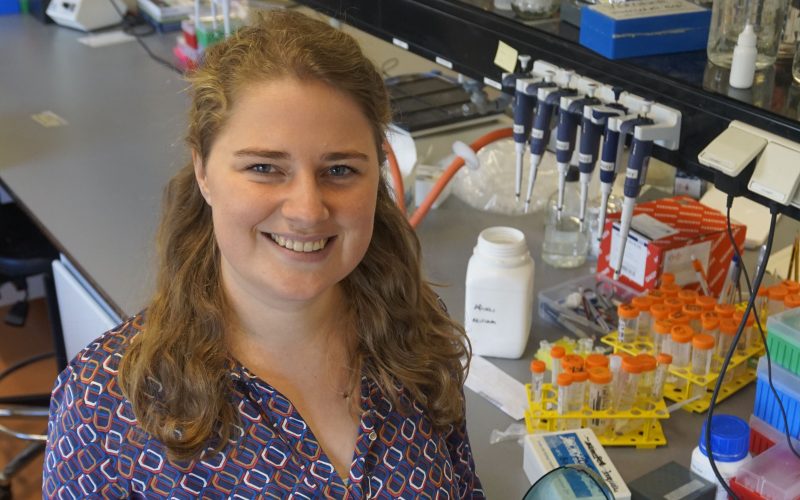
Astrid van der Geest
“We then zoomed in further on the organoid,” Astrid says, laughing. “As often happens in research, the experiments didn’t follow the organoids’ development chronologically, you always base your next study on the results of the previous one.” She tried to get a better picture of the cells by examining which RNA (which translates DNA into proteins) was floating around in them. “We wanted to see whether a certain type of cell was present in greater or lesser proportion. We specifically looked at people with ALS who have the C9ORF72 (C9) mutation: the most common mutation linked to ALS.”
The results showed that one cell type was less present: the deep-layer neurons involved in controlling the motor neurons, which in turn send movement signals to the body. “We also found that the communication between nerve cells was disturbed,” Astrid says.
For a long time, it was believed that people carrying the C9 mutation all had an equal chance of eventually developing ALS. But other research from the ALS Center showed that this is not the case. In some families, the risk seems higher than in others. “Based on signals from the clinic and other studies, I set up research where we made organoids from skin cells of people from families in which ALS occurs. We wanted to see whether brain organoids from C9 mutation carriers without ALS symptoms showed the same vulnerabilities as those with ALS.”
In the organoids, the researchers indeed found accumulations of the mutation, as well as other vulnerabilities, such as abnormal growth curves and reduced expression of certain genes. Astrid says: “The interesting thing was that we didn’t see these vulnerabilities in everyone.” This suggests that it might be possible to predict who is more likely to develop ALS later in life. Whether that is actually the case remains to be seen. Astrid explains: “In the future, we might be able to use brain organoids to gather additional information and make an individual risk assessment based on the vulnerabilities we see. If, one day, there’s a treatment for ALS, we could already know who to treat before symptoms appear: A step toward personalized medicine.”
Astrid emphasizes the importance of collaboration during her PhD journey. “Many of the perspectives in my research came from signals from the clinic or from other researchers. That so-called crosstalk between disciplines makes research so much more enjoyable. Even though you do lab work and don’t see patients yourself, collaboration with doctors and the involvement of the ALS Foundation Netherlands and the ALS Patient Association, makes it much more tangible what your research contributes to. You really feel the connection with families and loved ones. That’s incredibly valuable.”
You can read Astrid’s doctoral thesis here