Together with international partners from high- and low-resource settings, epidemiologist Esther van Kleef PhD (Epidemiology of Infectious Diseases, UMC Utrecht and Institute of Tropical Medicine, Antwerp) has received a JPIAMR grant of € 1.9 million to develop a low-cost surveillance approach to monitor antimicrobial resistance (AMR) outside the hospital setting in sub-Saharan Africa and predict AMR in clinical infections. This project is pioneering the use of metagenomics, which examines DNA from bacteria in pooled fecal samples to predict which antibiotics are still effective against serious infections.
In 2019, infections caused by bacteria that are no longer sensitive to antibiotics contributed to about 5 million deaths. The highest estimated mortality related to antimicrobial resistance (AMR) takes place in sub-Saharan Africa. Microbiology laboratories can investigate which bacteria cause disease in humans, check for AMR in these pathogenic bacteria, and collect information that can be used to make decisions about which antibiotics are best to use. However, in large parts of sub-Saharan Africa, there are few such laboratories, which are also expensive to set up and run.
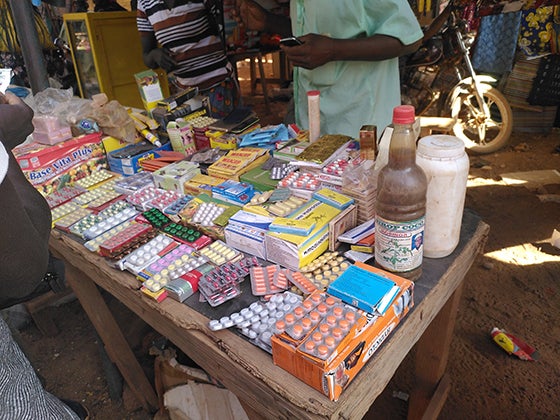
Alternative and cheaper approaches than standard laboratory tests are therefore needed to determine resistance patterns and guide which antibiotics are still appropriate. Many bacteria responsible for serious infections are already present in the intestines of future patients.
Consortium partners from the University of Oxford and KEMRI/Wellcome Trust Research Programme, Kenya have previously shown that for some bacterial species carried in the human intestine, it is possible to predict what resistance patterns are likely present in the event of serious infections by looking at the DNA of bacteria in pooled stool samples from hospital patients. In this study, which will be carried out in Kenya and Burkina Faso between 2024 and 2027, Esther and partners will investigate – with help of metagenomics – if this is also successful for other bacteria, and whether predicting resistance in severe infections is possible based on samples collected outside the hospital in villages, from human feces and from household environments. This will also allow to learn more how bacterial genes that cause resistance in bacteria spread between humans, and the environment. The consortium wants to conduct an economic evaluation to define how their approach can be translated to an efficient use of resources for AMR surveillance in settings, like many in rural sub-Saharan Africa – that lack microbiological diagnostic capacity.
This ZonMw grant was part of AMR Diagnostics and Surveillance 2023 call of the Joint Programming Initiative on Antimicrobial Resistance (JPIAMR) a global collaborative organization and platform, engaging 29 nations to curb AMR with a One Health approach.