PhD research by Julia Egido Egido (UMC Utrecht) has shown in in vitro studies that bacteriophages may act synergistically with certain antibiotics to kill bacteria. On the other hand, she found that the human complement system can inhibit certain phages in vitro which may compromise their antibacterial activity. These findings provide new insights that are helpful in the development of phage therapy.
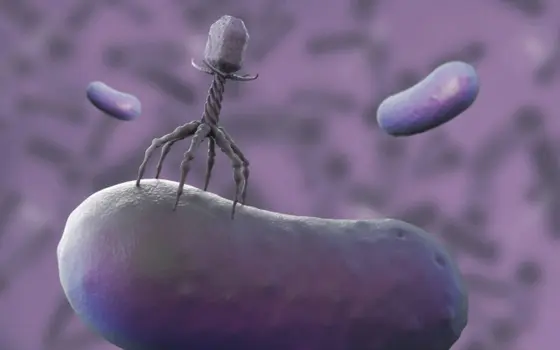
Antimicrobial resistance is becoming a greater problem in today’s society, leading to previously treatable infections becoming more dangerous. It is therefore important that the development of new treatment options is pursued. There are different strategies being investigated for this, but a major area of interest is the use of bacteriophages (phages). Phages are viruses which specifically target bacteria. They bind to the bacterium and reproduce inside it. This process results in bacterial death while new phages are released. These phages can then further attack the bacterial population. This makes bacteriophages an interesting and potentially safe therapeutic option due to their specificity towards bacteria, killing capacity and ability to self-amplify. One pathogen for which phage therapy can be particularly useful is Pseudomonas aeruginosa. In her PhD thesis, Julia Egido Egido (Department of Medical Microbiology, UMC Utrecht) and colleagues have investigated factors influencing the efficacy of therapeutic phages against this pathogen.
The investigators developed and validated a more rapid and less labor-intensive fluorescence assay to monitor phage activity against Gram negative bacteria in real time. Using this assay, they have evaluated the activity of phages in human serum and found that the complement system, an important agent of the innate immune system, can recognize and inhibit phages of a certain type called myophages, potentially compromising their antibacterial activity.
They also studied how phages can work together with antibiotics of certain classes to eliminate P. aeruginosa. The results showed that phages can act in a synergistic way with several different antibiotics, particularly the β-lactams meropenem and ceftazidime. The investigators hypothesize that these antibiotics might boost the amplification of phages within bacteria. Finally, Julia dove into the mechanisms of bacterial defense and resistance against phages, in a review that also discusses the clinical implications of these mechanisms.
Julia Egido Egido summarizes the main findings of her research: “Taken together, the work of my PhD thesis has provided new tools to study phage-bacteria interactions. Furthermore, we have generated knowledge about how therapeutic phages may be influenced by factors like the human immune system and antibiotic co-treatments. One conclusions that we can draw from this research is that it is crucial to select the optimal phages to maximize the chances of therapeutic success. Currently, phages are chosen for therapy mainly based on whether they can infect a given pathogenic bacterial strain. We think that it would be beneficial to take other factors into account, like how the patient’s immune system will affect them, what antibiotics are administered at the same time, and how resistance to these phages can develop. By expanding our knowledge on these topics, we hope to eventually be able to predict which phages are the most suited for each individual patient, thereby contributing to the design of better phage therapy strategies.”
Julia Egido Egido (1995, Zaragoza, Spain) defended her PhD thesis on April 2, 2024 at Utrecht University. The title of her thesis was “Understanding therapeutic phages – In vitro approaches to an improved strategy against bacterial pathogens”. Supervisor was prof. Suzan Rooijakkers PhD (Department of Medical Microbiology, UMC Utrecht). Co-supervisors were Pieter-Jan Haas MD PhD and Bart Bardoel PhD (both Department of Medical Microbiology, UMC Utrecht).