PhD research by Roos-Marijn Berbers at UMC Utrecht shows that immune dysregulation in patients with CVID comprises profound chronic activation of the immune system and dysbiosis of the respiratory and gut microbiota. Moreover, microbial dysbiosis may result in presence of specific pathogens that are associated with autoimmune disease, and which exacerbate the deregulation of the immune system resulting in clinical symptoms.
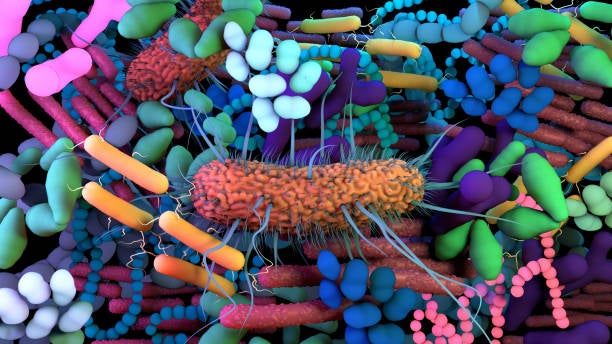
Common variable immunodeficiency (CVID) is an immune disorder that not only causes increased susceptibility to infection, but also to inflammatory complications such as autoimmunity, lymphoid proliferation and lymphoma. Recent findings implicate the microbiome as a driver of this systemic immune dysregulation. PhD student Roos-Marijn Berbers (Department of Rheumatology & Clinical Immunology and Department of Medical Microbiology, UMC Utrecht) investigated the role of gut and respiratory microbiota in inflammation and immune dysregulation in CVID.
While previous research has already demonstrated that Immunoglobulin A (IgA) plays a key role in homeostasis of the microbiome, Roos-Marijn Berbers showed in a cross-sectional study in patients with stable CVID that chronic lung disease was associated with IgA deficiency and important changes in the relative abundance of specific oropharyngeal bacterial taxa (as compared to healthy controls). Structural airway disease was associated with a higher abundance of Prevotella, Alloprevotella, and Selenomonas taxa, whereas interstitial lung disease was associated with a higher abundance of Streptococcus and a lower abundance of Rothia taxa These findings confirm that IgA is important for upper airway tract microbiota homeostasis and that IgA deficiency may result in changes of the microbial composition of the upper respiratory tract. However, if and how these findings relate to lower respiratory tract microbiota remains to be established.
In a cross-sectional study in CVID patients, Berbers also showed that disturbance of the gut microbiota composition contributes to inflammation in CVID patients with immune dysregulation (the more severe variant of CVID). The gut microbiota in this patient group was characterized by expansion of Enterobacteriaceae and bacterial invasion of colonic crypts in biopsies as compared to healthy controls. In addition, increased fecal bacterial load and decreased diversity were observed. Presence of Enterococcus gallinarum was associated with increased serum levels of inflammatory markers (e.g. IL-17A and IL-10). Moreover, exposure of monocytes to E. gallinarum supernatant resulted in increased production of IL-6 and a higher IL-6/IL-10 ratio. This study further supports the hypothesis that changes of the gut microbiota composition contributes to systemic inflammation in CVID. Therefore, E. gallinarum has been identified as a pathogen of interest in CVID with immune dysregulation.
Roos-Marijn Berbers concludes: “In my thesis we show that immune dysregulation in patients with CVID is a complex and heterogeneous disease that comprises profound chronic activation of the immune system and dysbiosis of the gut microbiota. In CVID, immune deficiency can result in microbial dysbiosis, including changes in the relative abundance of specific pathogens that are associated with autoimmune disease, which exacerbates the deregulation of the immune system resulting in clinical symptoms.”
Common variable immunodeficiency (CVID) is a rare, chronic immune disorder characterized by low antibody levels (specifically of immunoglobulins IgG, IgM and IgA). Symptoms include increased risk of (recurrent) infections, chronic lung disease, and inflammation and infection of the gastrointestinal tract. The underlying causes are largely obscure, but genetic factors have been identified as the cause of CVID in about 10 percent of patients. CVID has an estimated prevalence of about 1 in 50,000 in Caucasians, but seems less prevalent amongst Asians and African-Americans.
Roos-Marijn Berbers (1991, Amsterdam) defended her PhD thesis on September 21, 2021 at Utrecht University. The title of her thesis is “Microbiome and inflammation in antibody deficiency”. Supervisors were prof. dr. Rob Willems (Department of Medical Microbiology, UMC Utrecht) and prof. dr. Jaap van Laar (Department of Rheumatology & Clinical Immunology, UMC Utrecht). Co-supervisors were dr. Helen Leavis (Department of Rheumatology & Clinical Immunology, UMC Utrecht) and dr. Pauline Ellerbroek (Department of Internal Medicine, UMC Utrecht). Roos-Marijn Berbers works as a resident in internal medicine at the St. Antonius Hospital in Nieuwegein.