The feeling after receiving a nice Christmas present. The sensation after buying a new car, complete with all the associated innovative applications. This is how Gregor Krings and Mirella Molenschot respectively describe their first days after the installation of ultramodern 3D equipment in the cardiac catheterization room of the Wilhelmina Children’s Hospital (WKZ) reopened this week. “We can now take even sharper images and treat patients even more precisely and safely,” say the pediatric cardiologists.
For more than a decade, the WKZ has been the only medical center in our country where 3D images are taken of children with congenital heart defects before and during cardiac catheterization. By thus creating a “3-dimensional map” of their hearts and immediate surroundings, doctors know exactly what treatment is and is not possible. What’s more, even the patient’s parents are aware of this – and the child itself if it is old enough to understand it – because they are given a digital video of the internal situation to take home.
“Some children hold a talk at school about their heart defect and then show the video to their classmates,” says Gregor Krings, head of pediatric cardiology. “The picture is very clear: not black and white and with two dimensions, but true to life, i.e. in color and with three dimensions.”
But with medical equipment, it’s like with a smartphone or Ipad: after a while, the device starts to falter and it’s time for a more modern one. Mirella Molenschot: “We have been very happy with our 3D equipment for years. It is thanks to the old device that we have come so far with 3D imaging and that we can now share the many experiences with heart patients with doctors who treat children with other diseases. Think of surgical treatment of kidney and liver tumors at the Princess Máxima Center. Or the surgery of children with a faulty esophagus or trachea. Then we sit with other doctors in front of the computer, make 3D files of a CT image and look at the problem from all sides – as if we were holding it in our hands. But the new 3D equipment offers many more possibilities. Gregor, I and the third pediatric cardiologist who does pediatric cardiac catheterization have begun a journey of discovery to fine-tune these capabilities and become familiar with them.”
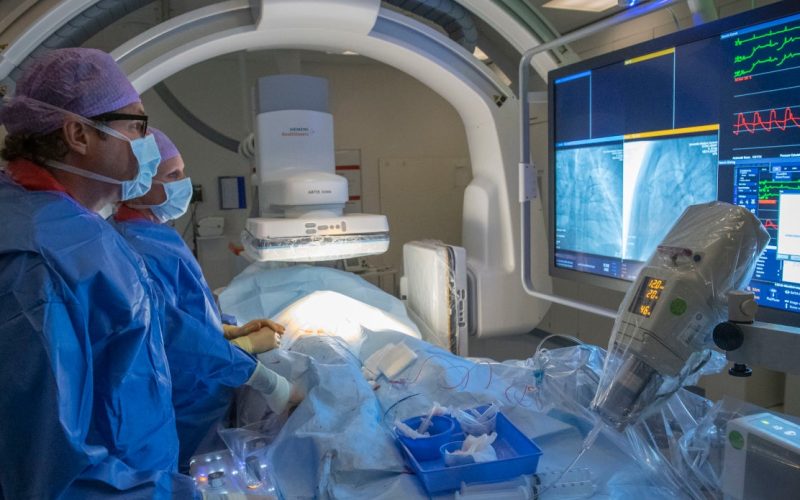
Better image quality, less burden on the patient and faster availability of the desired images. Those are the biggest benefits of the innovation, created by Siemens. Mirella: “Fewer images are needed to create a good 3D image, and the scan time of an image is also shorter: 3.8 instead of 5 seconds. This means that the patient is burdened less with X-rays and less contrast medium is needed. Furthermore, after the recordings, the current image appears on our screen earlier than before. In addition, the image is sharper ánd more details can be seen, so the 3D character is enhanced.” Gregor: “We were already rotating in the patient’s body, but now we are in the middle of it.”
Every year, pediatric cardiologists at the WKZ deploy cardiac catheterization on an average of 150 to 200 children with congenital heart defects. “For two-thirds of these boys and girls, we use 3D technology,” Gregor says. “This is by definition high-complex care. The patient lies while an X-ray tube rotates around him or her: within 3.8 seconds, the tube rotates 180 degrees. Within ten seconds, the system automatically generates the first 3D image. We edit that, think foreground and background, until we have the desired image in one to ten minutes.”
The pediatric cardiologist talks about “precise planning. He gives an example: “In Utrecht, we developed the oval stent technique, a metal tube that can be placed in a narrowed pulmonary artery, for example, to widen it. The stent is in a catheter inserted through a groin and then moved toward the heart. But you can’t just place a stent. You’ll first have to check in and around the heart to make sure you don’t damage the neighbors of the narrowed artery. Consider the airway, body artery and coronary artery. For example, if a stent flattens a coronary artery, the patient is at great risk of death. So it is essential to first understand and then act. That’s exactly where 3D technology helps. We can also make a 3D print of the heart prior to any cardiac catheterization to get an accurate picture. Then you have in your hands a one-to-one model of the patient’s heart.”
At the WKZ, precise planning and research go hand in hand so that innovations are developed at the 3D level and patient care improves ever so slightly. Gregor: “Suppose we are discussing the best possible treatment for a baby with a congenital heart defect. Nowadays, we can mimic blood flow in the process by applying ingenious technology such as Computational Fluid Dynamics. Not only do we visualize the heart in 3D, but we also see on the screen the consequences of a certain action on blood flow. How would the blood flow if we did this? And how could we ensure better blood flow?”
The more than a decade of 3D experience in children with congenital heart defects has also increased treatment options for boys and girls with other heart problems. Gregor: “A five-year-old girl loved horses. One time she was standing behind a horse and got a kick to her chest. She was in pain and was taken to the WKZ. On 3D images we saw a large tear on the outside of her large artery. The vein was not yet torn open. Then we first carefully studied the tear in 3D, considered the options and finally sealed the large artery with stents on the inside. The girl is completely healthy again.”
The fact that the WKZ can perform heart catheterizations at an increasingly higher level has the added benefit that more children can be spared open-heart surgery. There is no need to open their chests and connect them to a heart-lung machine. In addition, the patient recovers faster after cardiac catheterization than after open-heart surgery. Sometimes open-heart surgery is the best scenario but cannot be followed, for example because a patient is too frail. Then cardiac catheterization may be the only way to still give a child a chance of survival.