Clonal dissemination appears to be the major driver of the spread of one type of vancomycin resistance in Dutch hospitals, followed by horizontal plasmid-mediated dissemination. This study by investigators at UMC Utrecht demonstrates the feasibility of distinguishing between modes of dissemination with short-read data and provides a novel assessment method to estimate the relative contribution of nested genomic elements in the dissemination of vancomycin resistance.
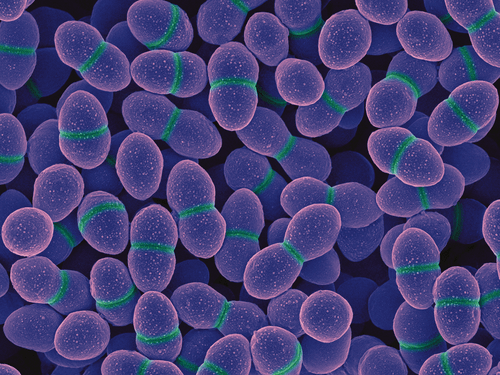
The bacterium Enterococcus faecium is a commensal of the gastrointestinal tract of animals and humans but can also cause hospital-acquired infections. The bacterium is often resistant against the glycopeptide antibiotic drug vancomycin. This has motivated the inclusion of E. faecium in the WHO global priority list of antibiotic-resistant bacteria for which effective new antibiotics are urgently needed. Vancomycin resistance can be conferred by the vanA gene cluster on the transposon Tn1546, which is frequently present in plasmids. The vanA gene cluster can be disseminated clonally but also horizontally either by plasmid dissemination or by Tn1546 transposition between different genomic locations.
Investigators at the Department of Medical Microbiology at UMC Utrecht performed a retrospective study of the genomic epidemiology of 309 vancomycin-resistant E. faecium (VRE) isolates across 32 Dutch hospitals (2012–2015). The study revealed that 59 percent of vancomycin-resistant Enterococcus (VRE) cases with a potential epidemiological link were unrelated, which was defined as VRE pairs with a distinct Tn1546 variant. Clonal dissemination accounted for 32 percent of cases in which the same sequence cluster and Tn1546 variants were identified. Horizontal plasmid dissemination accounted for 7 percent of VRE cases, in which they observed VRE pairs belonging to a distinct sequence cluster but carrying an identical plasmid and Tn1546 variant. The remaining 2 percent of cases were mixed and consecutive events of clonal and plasmid dissemination.
The authors conclude that in related VRE cases, the dissemination of the vanA gene cluster was dominated by clonal spread. However, they also identified outbreak settings with high frequencies of plasmid dissemination in which the spread of resistance was mainly driven by horizontal gene transfer. This study thus demonstrates the feasibility of distinguishing between modes of dissemination using short-read data and provides a novel assessment to estimate the relative contribution of nested genomic elements in the dissemination of vanA-type resistance.
Dr. Anita Schürch, assistant professor at UMC Utrecht and last author of the publication concludes: “Our analysis shows the importance of taking all nested genomic elements into account to effectively elucidate how resistance spreads in healthcare settings. This is fundamental to corroborate potential epidemiological links that could be neglected by uniquely considering strain relatedness. Only then, the effectiveness of current infection control policies to prevent antimicrobial resistance spread can be truly assessed.”
Arredondo Alonso S, Top J, Corander J, Willems RJL, Schürch AC. Mode and dynamics of vanA-type vancomycin resistance dissemination in Dutch hospitals. Genome Med 13, 9 (2021). https://doi.org/10.1186/s13073-020-00825-3