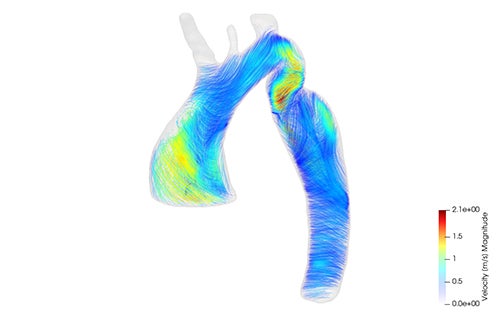
A 4D-MRI showing live blood flow in individuals with congenital heart defects. Both the pumping pattern and blood flow of the vessels as well as turbulence in the vessels. Then smart software is used to predict exactly what the best treatment is. These are the latest gadgets from the Center for Congenital Heart Defects UMC Utrecht.
Sometimes newborns have serious heart defects that require surgery immediately after birth. These are life-saving but major operations. The Center for Congenital Heart Defects is constantly looking for ways to improve these treatments. Not only for a better immediate effect, but also for a better life later.
“Heart defects are often located in the large vessels such as the pulmonary artery and body artery with many branches,” says Gregor Krings, head of the Center for Congenital Heart Defects at the Wilhelmina Children’s Hospital. “Then we want to know exactly what the anatomy of the heart and major vessels looks like. Imaging techniques in 3D and 4D are the basis for this. A 2D image of the heart is like a picture of a tree. With a 3D image, you can walk around the tree and see crooked branches from all sides.”
“Partly on this basis, we can optimally plan and safely perform a cardiac catheterization or heart surgery.” One step further is 4D technology, which is a moving 3D image. You watch, as it were, how the branches of a tree move in the wind. With 4D, the pumping pattern of the heart and the flow of the vessels become visible. “To determine whether or not an operation is necessary when a narrowing occurs, we look at the cross-sectional area of a lung or body artery and the blood pressure difference in the major vessels, among other things,” Gregor explains. “With the help of 4D techniques, we get additional information. Namely, with this we can visualize the degree of ‘turbulence’ of the blood circulation and its consequences.”
Physician-researcher Evangeline Warmerdam on the 4D-MRI: “With this technique, we can visualize the blood flow in detail. This makes constrictions more visible.” Her colleague Maartje Conijn, is mainly concerned with another, related, technique: Computational Fluid Dynamics (CFD). “With this, based on computer calculations, we can predict what the outcome of a treatment will be. So now you can calculate the best place for a stent, for example. That placement can also be tried out digitally, so you can see what the actual effect is before you actually place the stent.”
Thanks to these techniques, we have more information to arrive at the optimal treatment for patients. “Because there is more visibility into what is actually happening in the artery, we can place stents better than before. For example, we can make them bend exactly with the blood vessel. So the stent can be adapted to the artery,” says Evangeline.
A patient with a congenital heart defect is usually not repaired or finished after one operation. He remains a patient for life. After surgery on the aorta, for example, residual stenosis often remains (an aortic arch that is too narrow) due to scar tissue, for example. As a result, patients maintain symptoms such as headaches, high blood pressure, cardiovascular disease throughout their lives. They take medication for the rest of their lives. Maartje: “4D MRI and CFD not only help to properly map the original defect, but also to assess whether or not the residual symptoms will lead to complaints and can be treated.”