Current treatments to combat hypoxic-ischemic brain injury or encephalopathy of prematurity (i.e. brain injury due to extreme preterm birth) are very scarce. Therefore we are dedicated to develop new therapeutic neuroprotective and neuroregenerative strategies to improve outcome for these smallest of patients. We take a true bench-to-bedside approach by using clinically relevant cell- and animal-models to closely mimic brain injury in the human newborn and to test new treatment options via clinically applicable routes. We work in close collaboration with the clinical Department of Neonatology.
Developing Neuroprotective and Neuroregenerative Therapies for Neonatal Brain Injury
Current treatments to combat hypoxic-ischemic brain injury or encephalopathy of prematurity (i.e. brain injury due to extreme preterm birth) are very scarce. Therefore we are dedicated to develop new therapeutic neuroprotective and neuroregenerative strategies to improve outcome for these smallest of patients. We take a true bench-to-bedside approach by using clinically relevant cell- and animal-models to closely mimic brain injury in the human newborn and to test new treatment options via clinically applicable routes. We work in close collaboration with the clinical Department of Neonatology.
Advancing Intranasal Mesenchymal Stem Cell Therapy for Neonatal Brain Injury
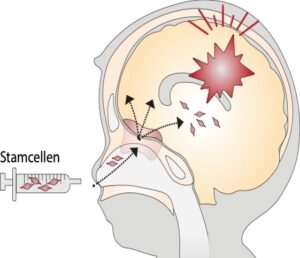
At present, one of our key focus points is developing intranasal mesenchymal stem cell (MSC) therapy from bench-to-bedside for neonatal brain injury. We study the migration of MSCs from the nose into damaged brain lesions, we focus on optimization strategies for cell-based therapy, and we explore mechanisms of neurorepair and stimulation of endogenous stem cell niches. Our previous research in this field has led to the first-in-human clinical trial in which safety of intranasal MSC application in term neonates with perinatal stroke has been explored (PASSIoN). We are currently also developing this therapy for encephalopathy of prematurity in animal models for fetal inflammation and fetal growth restriction.
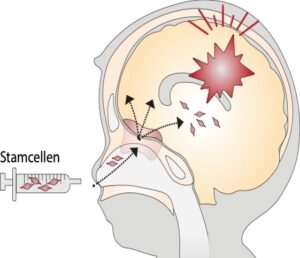
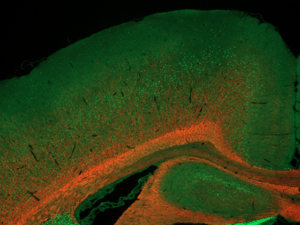
Image left: Illustration of intranasal application of mesenchymal stem cells to support endogenous neuroregeneration after neonatal brain injury.
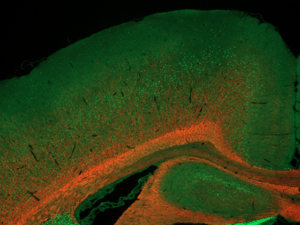
Image right: Will MSC treatment boost myelination (red, MBP) in brains of rats exposed to fetal growth restriction as a model for encephalopathy of prematurity? Deep cortical layers are stained for CTIP2 (green). Courtesy of Judit Alhama Riba.
Exploring Regenerative Strategies: Stem Cells, Growth Factors, and Nutritional Therapies for Neonatal Brain Injury
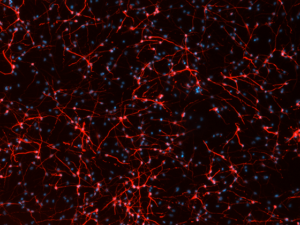
Besides MSCs, we also explore the use of neural stem cells and the use of MSC-secreted factors as regenerative strategies to improve neurodevelopment after neonatal brain injury. We investigate the anti-inflammatory and regenerative potency of MSC-derived extracellular vesicles in organoid models of brain injury. Additionally, we assess the regenerative effects of a crucial growth factor IGF1, which is depleted in preterm infants, highlighting it’s potency as a therapeutic strategy to treat encephalopathy of prematurity.
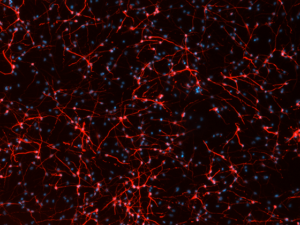
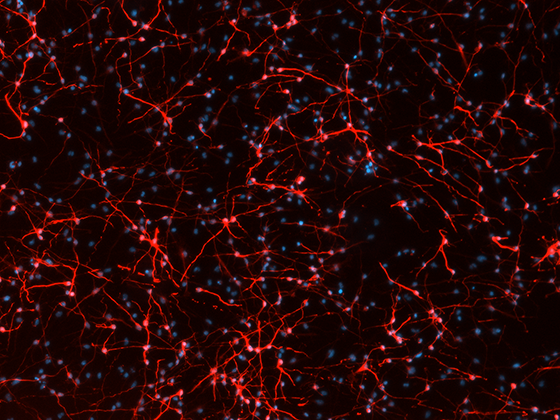
Image: Differentiation of neural stem cells into neuronal networks (red, betaIII-tubulin) in vitro is stimulated by mesenchymal stem cell-secreted factors. DAPI as nuclear counterstain. Courtesy of Sara De Palma.
 Prof. dr. Cora Nijboer
Prof. dr. Cora Nijboer