- ZonMw Meer Kennis, Minder Dieren (2023): Timing of fetal exposure to inflammation steers developmental brain injury in the newborn rat.
- ZonMw Meer Kennis, Minder Dieren (2023): Experimental models of Fetal Growth Restriction: a systematic review on neurological outcome.
- Valliant (2022): Schade aan de corpora mammilaria tijdens de geboorte: Is het te voorkomen?
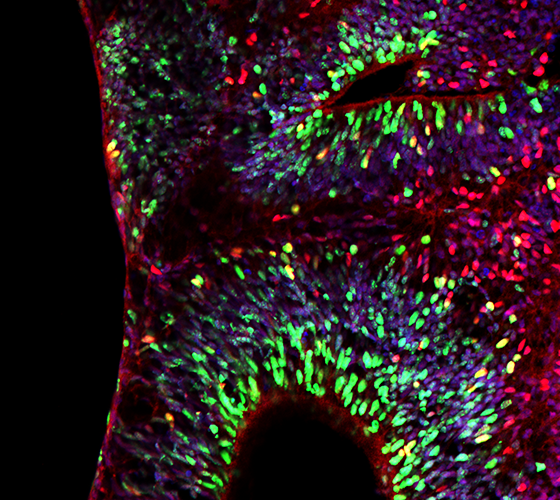
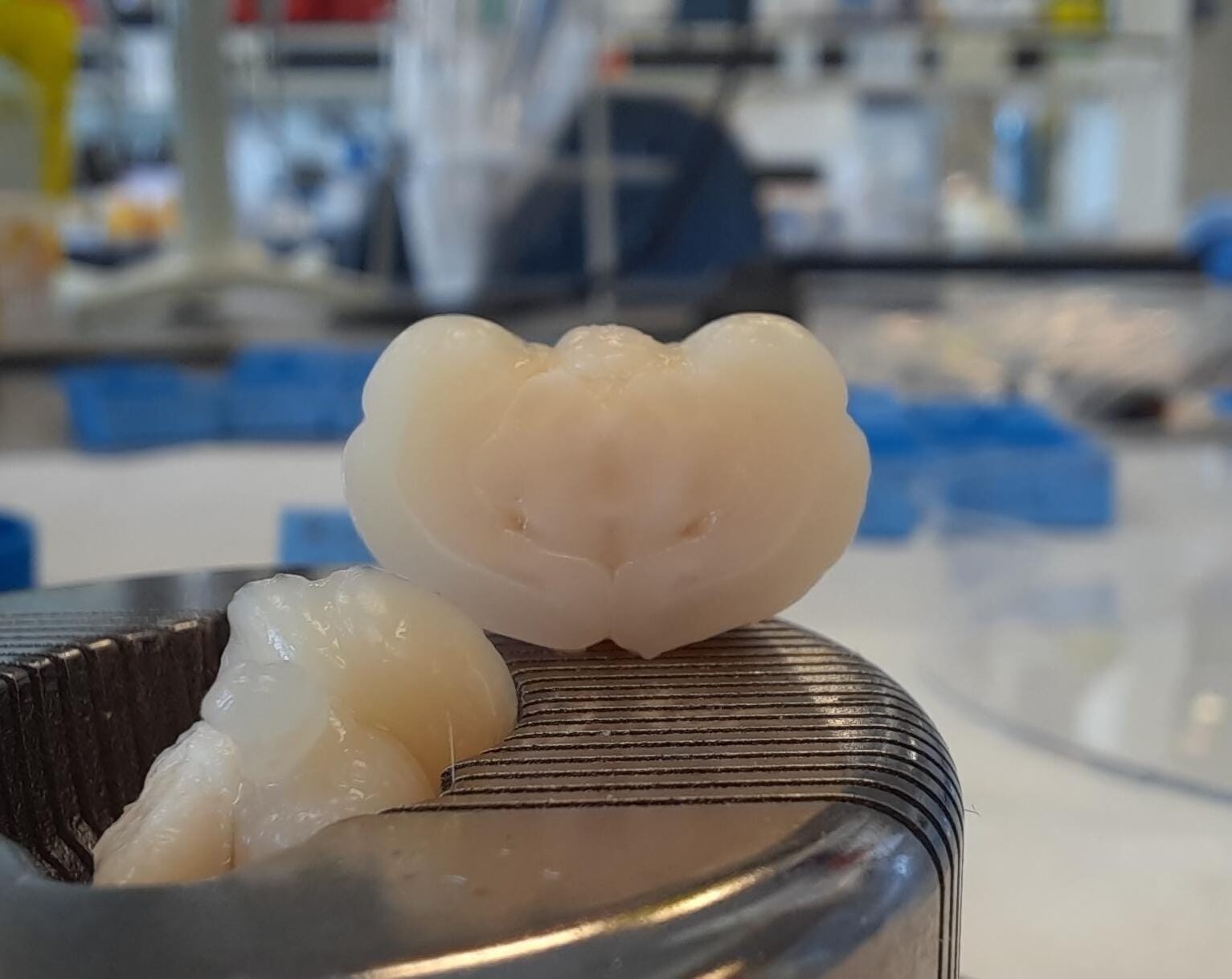
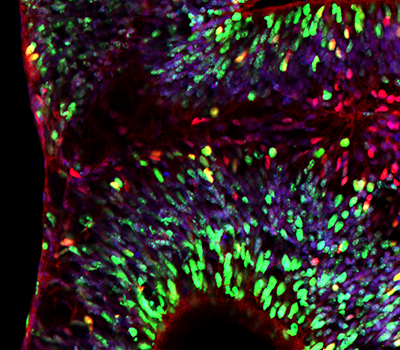
- 3V stimuleringsfonds (2020): Organoïde-model voor hersenschade bij te vroeg geboren kinderen (Myrna Brandt).
- ZonMw Meer Kennis, Minder Dieren (2018): Witte stof hersenschade in neonatale ratten leidt niet tot verminderde cognitieve vaardigheden op volwassen leeftijd (Erik van Tilborg).
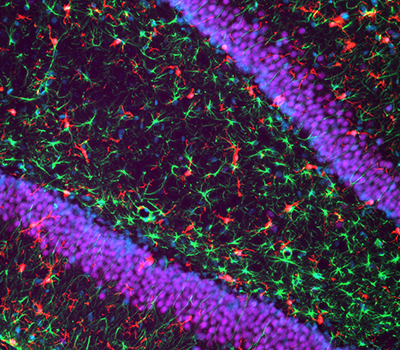
- Brain Foundation the Netherlands (2016), the Next Step program: Intranasal growth factor treatment: a novel strategy to repair the injured preterm brain.
- Brain Foundation the Netherlands (2014), fellowship: Mesenchymal stem cell therapy to repair white matter injury in the preterm neonatal brain: boosting oligodendrocyte differentiation and myelination.
- WKZ Research Funding (2013): A novel strategy to protect the preterm brain against perinatal white matter injury.
 Prof. Dr. Cora Nijboer
Prof. Dr. Cora Nijboer