We develop human airway epithelial cell models to understand why advanced therapies work for some individuals but not for others. Using stem/progenitor cells from nasal brushings, we grow personalized airway epithelial tissues that mimic a patient’s unique biology.
Chronic airway diseases such as cystic fibrosis (CF), primary ciliary dyskinesia (PCD), asthma, and bronchiectasis are highly heterogeneous and difficult to treat. Even among patients with the same mutation or diagnosis, variation in therapy response, inflammatory profile, or regenerative capacity is commonly observed. But why?
Airway Epithelial Cells as Memory Carriers
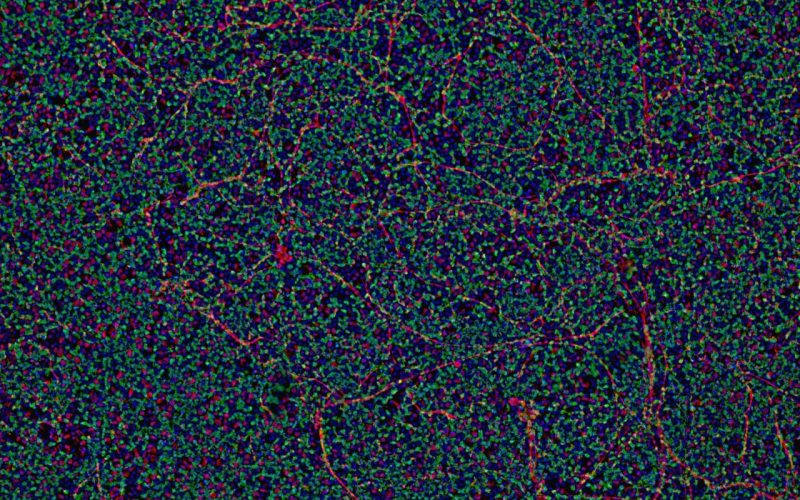
Our research group investigates the hypothesis that airway epithelial cells — particularly basal stem/progenitor cells — are not blank slates, but memory-bearing entities. These cells not only reflect an individual’s genetic makeup, but may also retain long-term traces of prior inflammation, disease exposure, or aging. Such traits can shape epithelial identity, plasticity, and responsiveness to treatment.
From Patient to Personalized Cultures
We use patient-derived airway cells from nasal brushings to generate personalized epithelial cultures. These models allow us to dissect donor-to-donor variation in a mechanistic way — with direct applications in therapy testing, immune–epithelial interaction studies, and future regenerative strategies.
Our research line currently focuses on three interrelated topics:
1. Stratifying therapy responses in airway models
We investigate how individual donor traits influence the response to CFTR modulators, gene therapies, and anti-inflammatory compounds. These insights are essential to improve the precision and predictability of treatment outcomes in chronic airway diseases.
2. Inflammatory memory and chronic epithelial remodeling
Chronic airway inflammation can leave a long-lasting imprint on basal stem/progenitor cells, altering how they differentiate and contribute to tissue architecture. This phenomenon, known as epithelial memory, may explain why some individuals develop persistent epithelial changes — such as excessive mucus production or impaired ciliation — particularly in conditions like type 2–high asthma, allergic CF, or post-viral airway disease.
3. Basal cell identity and regeneration potential beyond inflammation
Airway regeneration relies on basal stem/progenitor cells — but not all basal cells are the same. We study how donor-intrinsic factors such as age, genetic background, and regenerative potential shape basal cell identity and plasticity. These differences may determine how well epithelial tissues repair themselves after injury and which individuals are most suitable for future cell-based therapies.
Assistant Professor
Lab manager, technician
Technician
Technician
PhD student